In 1918 and 2020, Race Colors America’s Response to Epidemics

In American epidemics, race is a preexisting condition.
Whether it’s the influenza pandemic of 1918 or COVID-19 over a century later, race and ethnicity have been, and continue to be, enormous factors in determining whether people will receive medical attention when they become ill, and the sort of attention they will receive.
In “The 1919 Influenza Blues,” Essie Jenkins documented the toll the flu took on the country, noting that viruses don’t discriminate when it comes to their victims. She sang:
“People died everywhere
death went creepin’ through the air
and the groans of the rich
sure were sadBut it was God’s own mighty plan
He’s judging this old land
North and South, East and West
can be seenHe killed rich and poor
and he’s going to
kill some more …”
According to the Centers for Disease Control and Prevention estimates, the 1918 flu infected 500 million people worldwide and resulted in 50 million deaths around the globe, 675,000 of which were American. But while viruses don’t discriminate, people do. In cities across the nation, black people struck by the flu were often left to fend for themselves. They received substandard care in segregated hospitals, where they could be relegated to close quarters in basements, or they were only allowed admittance to black-only hospitals. Even in death, black bodies were neglected by white public infrastructure. In Baltimore that year, white sanitation department employees refused to dig graves for black flu victims after the city’s only black cemetery, Mount Auburn, could not accommodate any more graves.
“The mayor then had to appeal to the War Department, which is now called the Defense Department,” said Marian Moser Jones, a social historian and ethicist of public health at the University of Maryland. “The War Department sent 342 black soldiers, black American soldiers to do the task, which is very much in keeping with the way black soldiers were treated by the Army in the war. They were detailed to the worst duties, the most grueling labor details were the ones who were most often sent out to clean out the trenches after a battle and even exhume and rebury dead soldiers’ remains.
“It’s sort of a continuity from the war. The resources that were there, that were limited, the resources to address African American health and even death were overwhelmed in cities like Baltimore.”

In cities across the nation, black people struck by the flu were often left to fend for themselves. They received substandard care in segregated hospitals, where they could be relegated to close quarters in basements, or they were only allowed admittance to black-only hospitals. PUBLIC DOMAIN
The flu epidemic is inextricably linked to World War I. The first cases in the U.S. were identified in soldiers living in close quarters in Army barracks before heading to Europe to join the war, which the United States entered in April 1917. Even the name that we use to identify the disease, the “Spanish flu,” is inaccurate, according to historian Kenneth C. Davis, author of More Deadly Than War: The Hidden History of the Spanish Flu and the First World War.
“Fear driven by propaganda, censorship and lies were so much a powerful part of the spread of the Spanish flu. People were misled, often deliberately, by officials,” Davis said. “Newspapers were censored. The reason it is the Spanish flu is because of censorship. [During the war] Spain was a neutral country. It didn’t censor its news reports as rigorously as some of the warring countries did, so the first report of a massive epidemic comes out of Madrid in the spring of 1918 and that’s the reason it was reported by Reuters in London that Madrid was under a mass epidemic. That’s the reason it was called the Spanish flu. It certainly didn’t originate there.”
Today, in the age of COVID-19, it’s worth examining the social dynamics of 1918 and how their legacy continues to shape modern public health.
“A lot of my historian friends have a cottage industry now talking about the lessons learned. I’m a bit more cautious,” said Vanessa Northington Gamble, a medical doctor and professor of medical humanities and American studies at George Washington University. “Who you are — and I mean in terms of your race, your gender, where you live — will have a major role in how you experience COVID-19. It also will play a major role in the services that you get. … If there’s anything we can learn from the 1918 influenza epidemic, is that we really have to look at issues around race and class and racial and social inequities.”
RACE AND PATIENT CARE
When the flu epidemic of 1918 came to Chicago, black people were blamed, and that blame came directly from John Dill Robertson, the city’s commissioner of public health. It wasn’t just white medical officials who engaged in this sort of blame. Robertson had a tremendous influence on the way the Chicago Tribune covered migration, and there, the prejudice was plain. Even before the pandemic reached Chicago, the Tribune’s coverage of migration was alarmist.
A March 5, 1917, headline from the Chicago Daily Tribune, as it was known at the time, blared, Rush of Negroes to City Starts Health Inquiry.
The flu simply heightened those existing prejudices.

When the flu epidemic of 1918 came to Chicago, black people were blamed, and that blame came directly from John Dill Robertson, the city’s commissioner of public health. CHICAGO HISTORY MUSEUM/GETTY IMAGES
Half a Million Darkies from Dixie Swarm to the North to Better Themselves, the paper proclaimed July 8, 1918. In the corresponding article, reporter Henry M. Hyde laid out a series of pathologies: Black people moving to Chicago from the South, he wrote, “are compelled to live crowded in dark and insanitary rooms; they are surrounded by constant temptations in the way of wide-open saloons and other worse resorts.”
The reason for such ills wasn’t any innate inferiority that could be attributed to blackness. In an academic paper about Jim Crow and public health, Betsy Schroeder Schlabach, a professor of history and African American studies at Earlham College in Richmond, Indiana, explained how discriminatory housing policies created ghettos. Black people were relegated to limited parts of the city. Housing was overcrowded, and white landowners became slumlords, charging rents that were 15% to 25% higher for black tenants, and then refused to make needed repairs when asked.
“The way that the Tribune, especially, talks about disease is the same way they talk about the Great Migration: swarms of migrants coming to the city and bringing with them all sorts of disease,” Schroeder Schlabach said. “There’s similar ways that today we talk about the border or the way definitely [President Donald] Trump talks about immigration crisis and disease.”
Interestingly, the Nov. 2, 1918, edition of the Cleveland Advocate bore the headline: Flu Shuns Us, Says Health Doctor, referring to black people. The idea that black people were not getting the flu, or dying from it the way white people were, was a widely held belief at the time, Gamble said. Getting a clear picture of what black people experienced nationally during the flu pandemic is difficult. Gamble thinks that segregated black neighborhoods may have functioned as a makeshift quarantine. But it’s also likely that instances of black illness were underreported.
“The only year in the 20th century when black people in the USA had lower influenza mortality than white people was 1918,” researchers Helene Økland and Svenn-Erik Mamelund wrote in the International Journal of Environmental Research and Public Health. “One hypothesis is that black people, who mainly lived in the South and under miserable living and working conditions, cramped conditions, white racism and violence, and poor medical care, were less susceptible to the 1918 influenza pandemic autumn wave due to higher exposure to the less virulent spring and summer waves. However, this hypothesis, the mechanisms for the crossover in the role of race in 1918 pandemic mortality, and the subsequent return to the ‘normal’ pattern of higher black than white mortality in 1919, have received little attention in the literature, nor has this [or other] hypothesis been theoretically or empirically substantiated.”
Gamble was also circumspect about fully trusting black infection statistics. “I do not say it’s definitive. There’s some indications [that black people were less affected],” she said. “And black physicians believed it too. But even if the incidence was lower, the number of black people who got influenza in 1918 overwhelmed the health care and social services institutions that were available to black people. So black hospitals were overwhelmed. Black nurses were overwhelmed. Things such as the National Urban League, they had volunteers to go into homes to try and take care of people. They were overwhelmed, and especially because the black community, for the most part, was left on its own.”
Shroeder Schlabach found that Robertson’s public health edicts functioned as another layer of Jim Crow laws, limiting the movement of black Americans, and effectively quarantining them to ghettos on the city’s South Side. Public health officials became a de facto police force. Beginning in 1917, Robertson’s health department passed 75 regulations, regulating where people could drink water to where children could play. It also implemented mandatory reporting of flu cases.
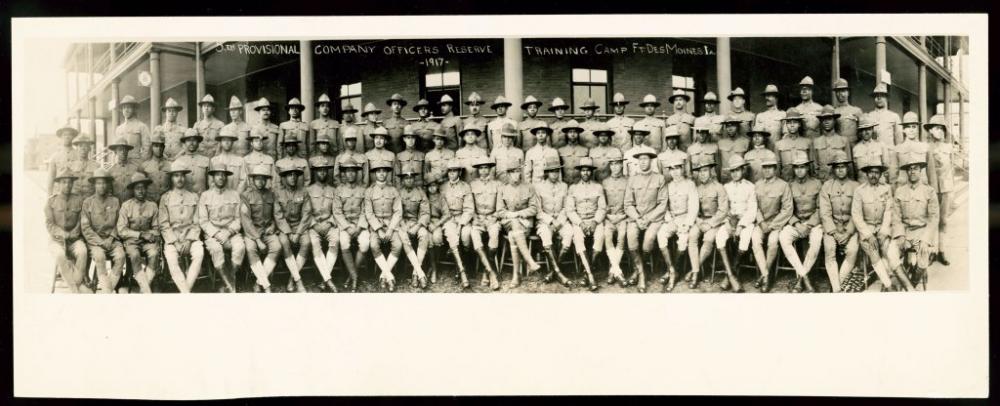
A picture of the black officers at Fort Des Moines, Iowa. This was the first time in U.S. history that the Army trained a cadre of African American officers, including 102 doctors. This picture does not capture the officers during the pandemic, but the pandemic is intertwined closely with the mass mobilization of troops for the war: Mobilized military men were the first population exposed to the pandemic — and died in droves. LIBRARY OF CONGRESS
“If you caught influenza, you were obligated to self-quarantine and then report that you had caught it to the Department of Public Health, and then they would come to your house and placard your house, like put a big red sign up on your house,” Schroeder Schlabach said. “That served to stigmatize disease. The Public Health Department sent visiting nurses on expeditions to find people who were sick. They would visit homes, and that resulted in about 40,000 visits [across the city] during the pandemic where nurses and public health officials could come into your house without your permission and ask if you were infected.
“What that does, especially for black households during the pandemic, is it takes away the sanctity of the home, giving the Public Health Department, who also had the power of the police, entering into your home. For the black family in early 20th-century Chicago, that’s a direct threat to their safety. These ordinances about mandated reporting of disease were the ones that functioned similarly to Jim Crow laws that regulated all facets of black life.”
Black people who were wealthy enough could visit a doctor in his office. Dr. Roscoe Giles, for example, placed ads in The Chicago Defender announcing his services. But for those who were less fortunate, Provident Hospital, the nation’s first black-owned and -operated hospital, was one of the few places where black people could be seen and treated. While black medical schools, such as Howard University Medical School, which grew out of the Freedmen’s Hospital in Washington, and Meharry Medical College in Nashville, Tennessee, were instrumental in turning out black physicians, Provident was crucial in training black nurses.
The Defender also ran columns by Dr. Wilberforce A. Williams advising black readers how to avoid the flu.
“He combines really practical advice about washing your hands, covering your mouth when you cough, but also, ‘If you want to be a good black citizen, donate to these things,’ or, ‘Live hygienically, and that means you can be a good person,’ ” Schroeder Schlabach said. “I found that to be a really interesting mix in his articles. In one article, he chastises a young mother who didn’t want to report that her child had contracted the disease because she feared social isolation. He just rakes her over the coals like, ‘This is foolish. You can’t put your pride before the well-being of the community.’ ”
Even as they were relegated to inadequate medical facilities, with black doctors and nurses facing shabby treatment and disrespect, black people still found ways to make the best of horrible situations.
“Black Chicagoans responded with innovation and tremendous grit and determination,” Schroeder Schlabach said. “At one point, the Public Health Department mandated that people needed to wear a mask. And what a group of black Chicago ladies do is that they start innovating with the masks and making them out of delicate lace and exquisite jewels. So even in the face of the pandemic, they were looking fabulous in these diamond-studded flu veils. Doctors and nurses just refused to accept any form of segregation. They’re more like icons. I see that as remarkable determination.”
RACE, PROFESSIONALISM AND MODERN INEQUALITY
The effects of America’s doctrine of separate and unequal life permeated everything during the 1918 flu epidemic. It not only shaped who received treatment and where, but also which people were deemed qualified to provide medical care.
In the midst of the first World War and the flu epidemic, there was a hope that black people could prove themselves as full Americans by serving their country, both in the medical field and in the military. The occupations, they hoped, would function as a “citizenship machine.”

Soldiers of the 369th regiment of the American Army in 1919 (Harlem Hellfighters) who won the Croix de Guerre for gallantry in action. From left to right in the front row: Pvt. Ed Williams, Herbert Taylor, Pvt. Leon Fraitor, Pvt. Ralph Hawkins. From left to right in the back row: Sgt. H.D. Prinas, Sgt. Dan Storms, Pvt. Joe Williams, Pvt. Alfred Hanley, Cpl. T.W. Taylor. PHOTO 12/ UNIVERSAL IMAGES GROUP VIA GETTY IMAGES
“It was W.E.B. Du Bois who really motivated African Americans to enlist and join the Army,” Davis said. “He thought this would really prove how they were loyal Americans who could make a great contribution to the war effort and to fighting. And some of the first American troops to go to France were African American troops, including the very famous group known as the Harlem Hellfighters.”
Yet white institutions like the American Red Cross (ARC) were loath to accept black nurses into their ranks to help with the war effort until the situation was so dire that they had no choice.
“Many African American women were rebuffed by ARC chapters when they sought to participate, and had to create their own alternatives for wartime voluntarism,” Moser Jones wrote in a case study of the American Red Cross’s response to the flu pandemic. “Similarly, black women seeking to enroll as ARC nurses met with frustration. During the war, the ARC served as the official recruiter of nurses for the U.S. Armed Forces. The nursing division, which required every ARC nurse to have completed three years of training in an accredited nursing school, enrolled 24,000 trained nurses. Trained black nurses, however, were rejected for service abroad, and were only enrolled as reserve members of the home defense program.”
“They were finally allowed to come in and treat white soldiers, but they were still of course living in segregated facilities,” Davis said. “So, even the angels of mercy taking care of these dying soldiers still had to confront the racism of the day.”
A job listing in the December 1918 Monthly Bulletin of the Department of Public Health and Charities of the City of Philadelphia was openly discriminatory:
There are four vacancies for assistant physicians at the Philadelphia Hospital for the Insane. Thirty-fourth and Pine Streets, two at a salary of $900 per annum and two at $720 per annum, including board, lodging, and laundry. Applicants must be white, twenty-one years of age, residents of Philadelphia, and licensed to practice in the State of Pennsylvania. These positions are open to both sexes. Successful candidates must reside at the hospital.
The Nov. 2, 1918, edition of The Chicago Defender reported that a black nurse named Olive Walker in Ohio was “denied the privilege of helping the Red Cross nurse committee to down the influenza epidemic at Hiram College. The dean of the college refused to allow her to serve when he became aware of her racial identity.” Lincoln Hospital in New York would hire black nurses, but not black physicians, Gamble said. And even the famous Dr. Giles of The Chicago Defender was asked to leave a new job at a tuberculosis sanitarium after six hours on the job. White patients didn’t want him to treat them.
Public health historians say that prejudice in American health care is once again at the forefront with the emergence of COVID-19. This time, Asians are the target of racialized scapegoating, from the Trump administration labeling COVID-19 the “Chinese virus” to Asian Americans being blamed for the pandemic’s presence in America.
“I called my mother, who works at a hospital in Northern California,” wrote Frank Shyong, a columnist for the Los Angeles Times. “I asked her to stay home, but her boss told her if she didn’t show up, she would lose her job. At work, patients sometimes refuse to be seen by her, because suddenly an Asian woman in a face mask is a threat.”
In November 1918, the Rev. Francis J. Grimke preached a sermon about the flu epidemic and what lessons could be gleaned from it. His words, delivered to the 15th Street Presbyterian Church in Washington, still hold tremendous relevance:
Jesus said, “The first and great commandment is, ‘Thou shalt love the Lord thy God with all thy heart, and with all thy soul, and with all thy mind, and with all thy strength.’ And the second is like unto it, ‘Thou shalt love thy neighbor as thyself.’ Upon these two commandments hang all the law and the prophets.” Race prejudice, colorphobia, runs directly counter to both of these great commandments. And, therefore, never mind what the white man may think of it, we see clearly what God thinks of it, and it is the estimate that He puts upon it that is to determine its character. Let us hope, therefore, not only for the sake of people of color, but also for the sake of the white people themselves that the great lesson as to the folly of race prejudice — of assuming that a white skin entitles one to better treatment than a dark skin, which this epidemic has so strikingly taught, may not be lost upon them. It is a lesson which for their own sake it is well for them to learn. It will be better for them here, and it will be better for them hereafter, if they learn it, and learn it well. And, of course, it will be better for us as a race in this country. It will remove out of the way some very serious obstacles to our progress, and will relieve us of many of the disagreeable things that we are at present forced to endure, though not without protest.
COVID-19 has not only brought interpersonal racism to the fore, but heightened the degree to which structural racism affects treatment and care.
Public defender Scott Hechinger and defense attorney Rebecca Kavanagh have pleaded with officials to release inmates as COVID-19 has spread through the close quarters of Rikers Island, New York City’s main jail complex. Similar situations exist in U.S. Immigration and Customs Enforcement detention facilities, where detainees are facing shortages of soap. Both places disproportionately house black and brown people.
“My worry is that there will be two standards of care, that incarcerated patients with one set of symptoms may be denied access to hospitals, even though in the community people with the same sets of symptoms do go to the hospital,” Dr. Homer Venters, the former chief medical officer for New York jails, told The Guardian. “And then that will lead to different rates of deaths and certainly to different rates of preventable deaths among people who are behind bars.”

In this Sept. 28, 1918, photo provided by the U.S. Naval History and Heritage Command, the naval aircraft factory float moves south on Broad Street escorted by sailors during a parade meant to raise funds for the war effort in Philadelphia. U.S. NAVAL HISTORY AND HERITAGE COMMAND/AP PHOTO
As with the 1918 flu, responses, or lack thereof, to COVID-19 have become tied up with patriotism and xenophobia in ways that exacerbate the spread of disease. In the midst of the 1918 pandemic, Philadelphia hosted a massive parade to sell war bonds to pay for the American war effort.
“There was enormous pressure,” Davis said. “If you didn’t buy the war bonds, you weren’t doing your part. You were a slacker. So 200,000 people go out, even though the health department knows that the virus is in and around Philadelphia, on the Navy bases, and they were going to have this parade and soldiers and sailors were going to be marching in the parade. Two days after that parade, every hospital bed in Philadelphia was filled and it was a complete disaster and it was a disaster because the authorities ignored the advice not to cancel this parade.”
In a live chat with constituents on Facebook, Tate Reeves, the governor of Mississippi, explained his opposition to giving official orders to the public to implement COVID-19 quarantines. “Eric Worth [a constituent] says ‘China did a lockdown and it was good for them. Why can’t Mississippi?’ Well, Eric, I’m going to tell you that Mississippi is never going to be China,” Reeves said. He has since given a shelter-in-place order to one county in the eastern part of the state, but insisted that a statewide shelter-in-place order was “not sustainable.”
In 1918, “things like the war effort and paying for the war and patriotism and support for the war, really outdid the concern for public health,” Davis said. “They were so interested to keep the troops going to Europe that they kept filling these ships up with sick men and these ships became what were called floating coffins. So, that’s a really important lesson as well. Misplaced priorities. When you place things like the economy over the public health, you do so at grave peril to many, many people.”
Soraya Nadia McDonald is the culture critic for The Undefeated. She writes about pop culture, fashion, the arts, and literature. She's based in Brooklyn. She has previously written for the Washington Post, the Los Angeles Times and the Colorado Springs Gazette. She is the 2020 recipient of the George Jean Nathan Award for Dramatic Criticism, a major award for writers on American theater. The prize committee includes the heads of the English departments at Cornell, Princeton and Yale universities and a member of each school’s theater faculty. George Jean Nathan (1882-1958) was a prominent American critic who published 34 books on the theater and co-edited, with writer H.L. Mencken, two influential 20th century magazines: The Smart Set and The American Mercury.
