Closing Medicaid Coverage Gap Would Help Diverse Group and Narrow Racial Disparities
The 2.2 million uninsured adults with incomes below the poverty line who were caught in the Medicaid “coverage gap” in 2019 are a varied group — they’re essential workers, parents caring for children, older and younger adults, and diverse in terms of race and ethnicity — but they all have something in common. They live in states that have failed to adopt the Affordable Care Act’s (ACA) Medicaid expansion, even with significant federal financial incentives, leaving this group with no pathway to affordable coverage.
States that haven’t implemented expansion should do so, and to account for states that won’t, Congress should act on calls from Senators Warnock and Ossoff and over 60 civil rights and other organizations to close the coverage gap by creating a federal fallback.
Adults in the coverage gap have incomes below the poverty line, which is too low to qualify for subsidized health insurance coverage in the ACA marketplaces, yet they don’t qualify for Medicaid under their states’ rules. As enacted, the ACA extended Medicaid coverage to adults with incomes up to 138 percent of the poverty line, with subsidized marketplace coverage available to those with higher incomes. However, the Supreme Court allowed states to choose whether to expand Medicaid, creating a coverage gap for people with incomes below the poverty line in the 12 states that haven’t expanded. These states’ income eligibility rules for Medicaid are stringent; the median state caps eligibility for parents at about 40 percent of the federal poverty line, or just $8,800 in yearly income for a single caregiver of two children. Generally, adults without children are ineligible for Medicaid in these states, regardless of how low their incomes are.
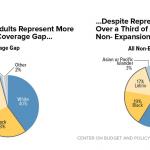
Extending health insurance to people in the coverage gap squarely benefits people with incomes below the poverty line who are uninsured and lack any access to affordable coverage.Extending health insurance to people in the coverage gap squarely benefits people with incomes below the poverty line who are uninsured and lack any access to affordable coverage. Some 60 percent of people in the gap in 2019 were people of color, reflecting long-standing racial and ethnic disparities in health care access that coverage extensions would do much to address.
And it would improve health care access for people who are in the coverage gap because of their employment challenges and caregiving responsibilities. Half of the coverage gap population worked in 2019, but much of the population experiences structural barriers to finding consistent work; their jobs are disproportionately less likely to offer health insurance; and their incomes fluctuate, which can put parents (who qualify for Medicaid in non-expansion states if their incomes are very low) into and out of eligibility. One in 3 people in the gap were parents with children at home. Research shows that extending coverage to parents increases enrollment among eligible children, so closing the coverage gap for adults would lead to coverage gains for children as well.
Who Is in the Medicaid Coverage Gap?
We estimate that 2.2 million adults aged 19 to 64 fell in the coverage gap in 2019 among the 12 non-expansion states. Our estimates are based on the 2019 American Community Survey, the most recent year of this survey available, and all estimates unless otherwise noted are for 2019. These data were collected prior to the pandemic and accompanying recession, and it is likely that accounting for job and income losses during the pandemic would lead to a larger estimate of the population in the coverage gap.
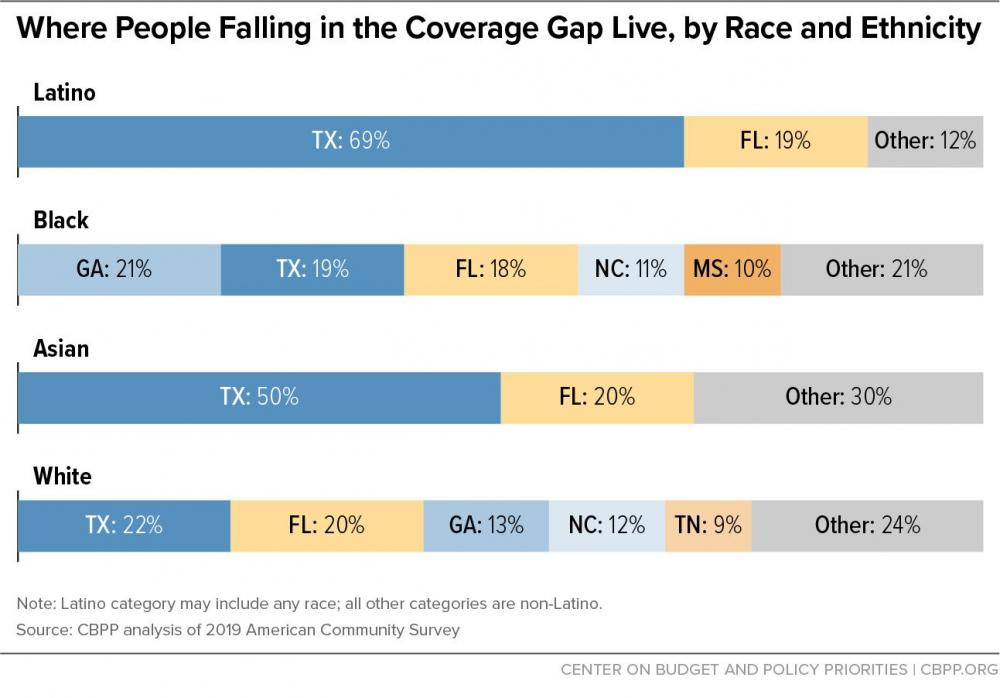
Across the 12 non-expansion states, those in the coverage gap were split almost evenly between women and men, and they spanned the 19-to-64 age spectrum of adults covered under expansion. About half of adults in the coverage gap were over 35, including about a quarter who were 50 to 64. (See Appendix I, Table 1, and Appendix II for our methodology.) Among those who were middle-aged and older, women comprised a slight majority, while most of those aged 19 to 34 were men.
Those in the coverage gap were disproportionately people of color. Most were in the labor force, roughly half were employed, and 1 in 3 were parents with children at home. Over half a million workers in the coverage gap were employed in front-line or essential industries, and about 15 percent of adults had a disability.
While we estimate that 2.2 million adults fell in the coverage gap in 2019, fluctuations in income and other eligibility criteria mean that many more people find themselves in the coverage gap over the course of a year. One study found that in a one-year period, low- and moderate-income households typically experienced more than five months in which their income fluctuated by more than 25 percent above or below their monthly average. Transitions into and out of Medicaid coverage are also frequent. For example, 13 percent of non-elderly adults with Medicaid coverage in January 2018 had lost coverage and become uninsured at least once by the end of the year.
Coverage Gap Exacerbates Racial and Ethnic Disparities
The COVID-19 pandemic has highlighted and exacerbated long-standing racial, economic, and health system inequities. People of color are disproportionately likely to lack access to care and have faced higher risks for COVID infection, hospitalization, and death. The ACA helped reduce disparities in health insurance coverage among states that expanded, but the coverage gap worsens these disparities by disproportionately denying coverage to people of color. While people of color comprised 41 percent of the adult, non-elderly population in non-expansion states, they made up 60 percent of people in the coverage gap, including 28 percent who are Latino and 28 percent who are Black. (See Figure 1.)
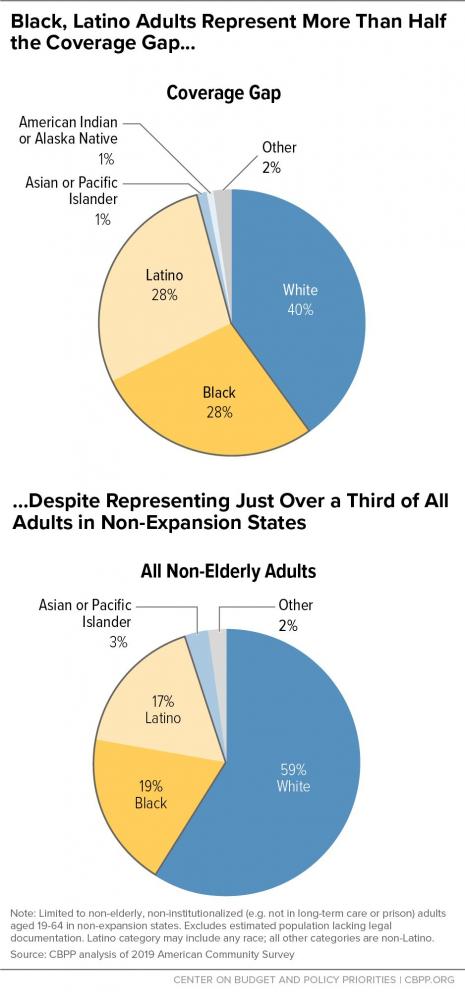
The vast majority of people in the coverage gap in 2019 lived in Southern states, with variations in racial and ethnic distributions. In Texas people of color made up 74 percent of those in the coverage gap, with Latino adults alone comprising 55 percent. In Mississippi most of the coverage gap population was Black, and in both Georgia and South Carolina it was more than 40 percent Black. (See Figure 2 and Appendix I, Table 2.) Over 70 percent of Asian adults and 88 percent of Latino adults in the coverage gap lived in Texas and Florida.
Most Adults in Coverage Gap Work or Are Caregivers; Many Are Disabled
Most adults in the coverage gap work or have caregiving responsibilities. Though by definition all adults in the coverage gap have incomes below the poverty line, 62 percent were in the labor force (that is, either working or available and actively looking for work) and about half — well over 1 million people — were employed in 2019. (See Figure 3 and Appendix I, Table 4.) In addition to facing inconsistent work opportunities as noted above, many in this group worked in low-wage jobs, which have accounted for a disproportionate share of the job losses due to the pandemic and downturn. Medicaid expansion, meanwhile, has been shown to improve people’s employment prospects.
Approximately 3 in 10 adults in the coverage gap were parents with children at home, and about one-third of these parents had a child under the age of 5. (See Figure 3 and Appendix I, Table 5.) The pandemic’s strain on caregivers and in turn on their children has been alarmingly high, making affordable health coverage key for both these groups.
More than a third of all adults in the coverage gap were women of reproductive age (See Appendix I, Table 5). If they become pregnant, these women can apply for pregnancy coverage. But coverage wouldn’t start until they’re determined eligible for Medicaid, which means they wouldn’t be covered before they became pregnant and during the first months of pregnancy and could miss out on services like preconception health counseling and early prenatal care. An Oregon study found that Medicaid expansion was associated with an increase in early and adequate prenatal care.
Medicaid expansion also provides an important pathway to coverage for people with disabilities. Nearly a quarter of non-elderly adult Medicaid enrollees had a disability, and most of them did not qualify for Medicaid through a disability pathway such as receipt of Supplemental Security Income (SSI). That’s because many people with a disability don’t meet strict state or federal standards for disability. Instead, most Medicaid enrollees with disabilities are eligible based on their income; for many this eligibility depends on their state’s Medicaid expansion decision. We estimate that there were approximately 324,000 uninsured adults in the coverage gap who had disabilities in 2019, or roughly 15 percent of the total coverage gap population. (See Appendix I, Table 6.) Among them, 7 percent had a serious cognitive difficulty, and more than 6 percent had difficulty with basic physical activities such as walking, climbing stairs, carrying, or reaching.
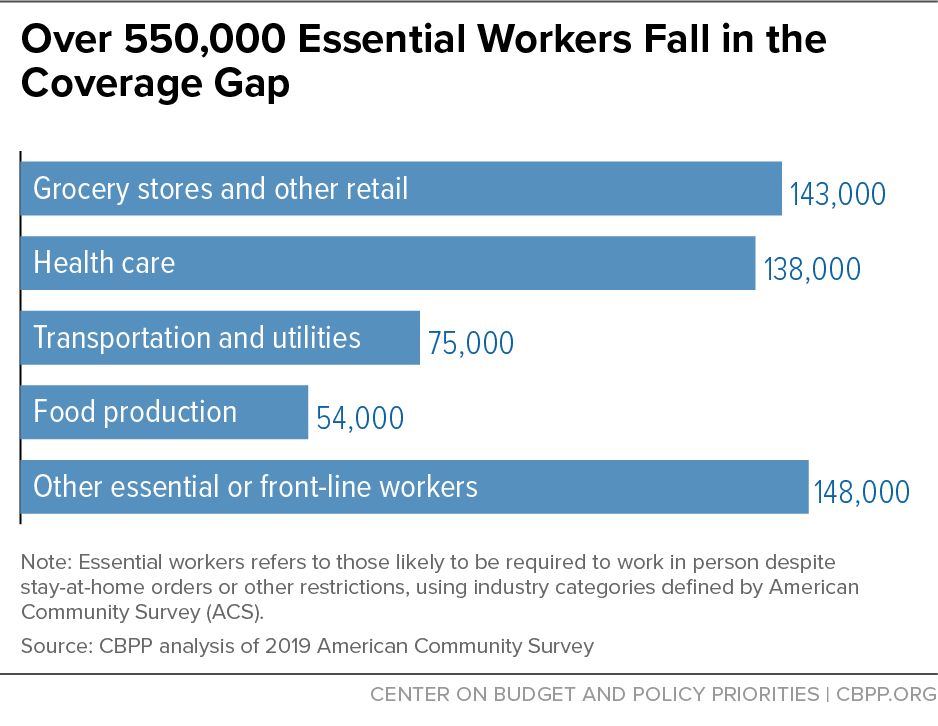
Over Half a Million People in Essential or Front-Line Industries Fall in Coverage Gap
During the COVID-19 pandemic, even as millions of people work in jobs that allow them to stay at home, millions of other front-line or essential people went to work (and continue to go to work) in person as health care workers, bus drivers, grocery store workers, food production workers, and other jobs that people rely on. Expansion states cut the uninsured rate for these workers by half from 2013 to 2019, double the reduction in non-expansion states, making these states better prepared for the pandemic and economic downturn.
Over 550,000 essential workers fell in the coverage gap in 2019. When the pandemic hit, such workers were left with no access to affordable coverage even as they risked their safety providing essential goods and services. Among those in the gap in 2019, 138,000 were health care workers and 143,000 were employed at grocery stores and in other front-line retail industries. They were concentrated in the largest coverage gap states, with 209,000 in Texas and 98,000 in Florida. (See Figure 4 and Appendix I, Table 3.) The industry distribution of these workers varied across states, with health care workers comprising the largest group in Texas and grocery store and other front-line retail workers making up pluralities in Florida, Georgia, and North Carolina.
Closing the Coverage Gap Would Improve Health and Financial Security
A large body of research demonstrates that Medicaid expansion increases health insurance coverage, improves access to care, provides financial security, and improves health outcomes.
Medicaid Expansion Improves Coverage and Access to Care
States that expanded Medicaid have seen significantly greater reductions in uninsured rates than states that failed to expand. In 2019 the uninsured rate among low-income, non-elderly adults had fallen to roughly half of the pre-ACA rate in expansion states, from 35 percent in 2013 to 17 percent in 2019. Non-expansion states experienced a much smaller reduction in the uninsured rate among this group, falling from 43 percent in 2013 to 34 percent in 2019. The Kaiser Family Foundation estimates that if the 12 remaining non-expansion states expand Medicaid, 4 million uninsured adults would become eligible for Medicaid coverage, equivalent to 36 percent of the uninsured non-elderly adult population in these states.
Medicaid expansion affects children’s levels of health coverage. Research shows that extending coverage to parents increases enrollment among eligible children. In Medicaid expansion states, more than 700,000 children gained coverage from 2013 to 2015 — more than twice as many as in non-expansion states. Medicaid expansion results in higher utilization of well-child visits, which links children to needed care. Young children without access to primary care may not have a pediatrician to track developmental milestones in growth or in walking and talking. Children enrolled in Medicaid benefit from greater access to dental care, eyeglasses, immunizations, asthma care, and pediatric check-ups as compared to uninsured children. Proper healthcare in childhood improves health outcomes as children reach adulthood and beyond.
Medicaid Expansion Prevents Premature Deaths and Protects Against Financial Insecurity
People in the coverage gap are at greater risk of preventable premature deaths. Medicaid expansion increases the use of preventative care and significantly reduces the utilization of emergency care, which results in earlier detection of cancers and more effective treatment of chronic illnesses. A recent study published in the Quarterly Journal of Economics found that Medicaid expansion saved the lives of at least 19,200 adults aged 55 to 64 between 2014 and 2017. Conversely, 15,600 older adults died prematurely as a result of some states’ decisions not to expand. This study examined only the first three years of expansion and found that the impact of expansion on mortality increased each year. Moreover, the study only examined the impact of premature deaths on older adults, not on the full population. The time since expansion has more than doubled since the study period, so the number of lives saved by expansion today is likely far greater.
Those in the coverage gap are also more susceptible to medical bankruptcy. Medicaid expansion is a powerful tool against financial hardship and bankruptcy as it protects beneficiaries from catastrophic out-of-pocket medical costs. In its first two years, Medicaid expansion led to a $3.4 billion reduction in medical debt sent to collections and 50,000 fewer bankruptcies nationwide. Charity care and bad debt among hospitals fell by $8.6 billion (23 percent) from 2013 to 2015, with declines among states that expanded Medicaid several times larger than for those that did not.
End Notes
Letter from Senators Raphael Warnock and Jon Ossoff to Senate Majority Leader Charles Schumer and Minority Leader Mitch McConnell, May 26, 2021, https://www.warnock.senate.gov/wp-content/uploads/2021/05/5.26.21-Medicaid-Expansion-Letter-.pdf; letter from Leadership Congress on Civil and Human Rights, May 27, 2021, http://civilrightsdocs.info/pdf/policy/letters/2021/052421-Medicaid-Coverage-Gap-Letter-FINAL.pdf.
The population in the coverage gap differs from estimates of the population that would gain health coverage if Medicaid were expanded in all states. The latter is an estimate of coverage (as opposed to eligibility) and would include people with incomes between 100 and 138 percent of the poverty line who are currently eligible for marketplace financial assistance but are not enrolled, as well as uninsured children who are currently eligible for subsidized coverage and would enroll if Medicaid expanded to cover their parents. The Urban Institute estimates that if the 12 states that have not enacted expansion were to expand in 2020, the net reduction in the uninsured would be approximately 4 million.
Adults with incomes between 100 and 138 percent of the poverty line were made eligible under the ACA for both Medicaid and marketplace coverage, but they are generally not eligible for federal subsidies for marketplace coverage when Medicaid is available.
A notable exception is Wisconsin, which extends Medicaid eligibility to adults up to 100 percent of the poverty line through a waiver and is therefore not included in coverage gap estimates. The 2021 federal poverty guideline for a family of three is $21,960 for the 48 contiguous states and the District of Columbia.
Anthony Hannagan and Jonathan Morduch, “Income Gains and Month-to-Month Income Volatility: Household Evidence from the U.S. Financial Diaries,” March 16, 2015, https://www.usfinancialdiaries.org/paper-1.
CBPP analysis of 2018 Medical Expenditure Panel Survey.
Sebastian Romano et al., “Trends in Racial and Ethnic Disparities in COVID-19 Hospitalizations, by Region – United States, March-December 2020,” Centers for Disease Control and Prevention, April 16, 2021, https://www.cdc.gov/mmwr/volumes/70/wr/mm7015e2.htm?s_cid=mm7015e2_w.
Jesse Cross-Call and Matt Broaddus, “States That Have Expanded Medicaid Are Better Positioned to Address COVID-19 and Recession,” CBPP, July 15, 2020, https://www.cbpp.org/research/health/states-that-have-expanded-medicaid-are-better-positioned-to-address-covid-19-and.
CBPP analysis of 2019 American Community Survey. Estimates exclude the estimated population lacking legal documentation and the institutionalized population.
For example, majorities of working people who gained coverage through the Medicaid expansion in Ohio and Michigan reported that it made them better at their jobs or made it easier for them to keep working. Ohio Department of Medicaid, “Ohio Medicaid Group VIII Assessment: A Report to the Ohio General Assembly,” January 2017, http://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Assessment.pdf. See also Kara Gavin, “Medicaid Expansion Helped Enrollees Do Better at Work or in Job Searches,” University of Michigan Health Lab, June 27, 2017, http://labblog.uofmhealth.org/industry-dx/medicaid-expansion-helped-enrollees-do-better-at-work-or-job-searches.
Claire Zippel and Arloc Sherman, “Bolstering Family Income Is Essential to Helping Children Emerge Successfully From the Current Crisis,” CBPP, updated February 25, 2021, https://www.cbpp.org/research/poverty-and-inequality/bolstering-family-income-is-essential-to-helping-children-emerge.
S. Marie Harvey et al., “Impact of Medicaid expansion in Oregon on access to prenatal care,” Preventive Medicine, Vol. 143, February 2021, https://www.sciencedirect.com/science/article/abs/pii/S0091743520303911?via%3Dihub.
MaryBeth Musumeci and Kendal Orgera, “People with Disabilities Are At Risk of Losing Medicaid Coverage Without the ACA Expansion,” Kaiser Family Foundation, November 2, 2020, https://www.kff.org/medicaid/issue-brief/people-with-disabilities-are-at-risk-of-losing-medicaid-coverage-without-the-aca-expansion/.
CBPP analysis of American Community Survey.
See Appendix II for our definition of front-line or essential industries.
CBPP analysis of 2019 and 2013 American Community Survey.
This includes 2.2 million uninsured adults in the coverage gap and an additional 1.8 million uninsured adults between 100 and 138 percent of the poverty line who are eligible for marketplace coverage but are not eligible for Medicaid. Rachel Garfield, Kendal Orgera, and Anthony Damico, “The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid,” Kaiser Family Foundation, January 21, 2021, https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/.
Julie Hudson and Asako Moriya, “Medicaid Expansion For Adults Had Measurable ‘Welcome Mat’ Effects on Their Children,” Health Affairs, September 2017, https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.0347?journalCode=hlthaff.
Maya Venkataramani et al., “Spillover Effects of Adults Medicaid Expansions on Children’s Use of Preventative Services,” Pediatrics, November 13, 2017, https://pediatrics.aappublications.org/content/early/2017/11/09/peds.2017-0953.
Julia Paradise, “The Impact of the Children’s Health Insurance Program (CHIP): What does the Research Tell Us?” Kaiser Family Foundation, July 17, 2014, https://www.kff.org/report-section/the-impact-of-the-childrens-health-insurance-program-chip-issue-brief/.
Samantha Artiga and Petry Ubri, “Key Issues in Children’s Health Coverage,” Kaiser Family Foundation, February 15, 2017, https://www.kff.org/medicaid/issue-brief/key-issues-in-childrens-health-coverage/.
Sarah Miller, Norman Johnson, and Laura Wherry, “Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data,” Quarterly Journal of Economics, January 30, 2021, https://doi.org/10.1093/qje/qjab004.
Kenneth Brevoort et al., “Medicaid and Financial Health,” National Bureau of Economic Research Working Paper 24002, November 2017, https://www.nber.org/system/files/working_papers/w24002/w24002.pdf.
Gideon Lukens, “Medicaid Expansion Cuts Hospitals’ Uncompensated Care Costs,” CBPP, April 20, 2021, https://www.cbpp.org/blog/medicaid-expansion-cuts-hospitals-uncompensated-care-costs.
Wisconsin extends Medicaid eligibility to adults up to 100 percent of the poverty line through a waiver. Therefore, Wisconsin has no coverage gap population and is not included in estimates.
Areas of Expertise
Recent Work:
-
Closing Medicaid Coverage Gap Would Help Diverse Group and Narrow Racial Disparities
-
Recovery Legislation Should Build On Affordable Care Act Improvements in Coverage for Adults Over 55
Recent Work:
The Center on Budget and Policy Priorities is a non-partisan research and policy institute which works at the federal and state levels on fiscal policy and public programs that affect low- and moderate-income families and individuals. Donate
