The Other Abortion Pill Option

Today, the Supreme Court is set to rule in the medication abortion case. The legal, medical, and public health implications of this case are huge.
But regardless of what they rule, a really important piece of the story has gotten little attention the past few weeks: even if mifepristone is severely restricted, we have another option.
The other option
For a medication abortion in the U.S., patients are given two pills: mifepristone (“mife”) followed by misoprostol (“miso”).
The legal cases have focused solely on the first medication: mife. This is because mife was specifically approved by the FDA in 2000 for abortions, to be used followed by miso.
Miso, on the other hand, was approved in 1988 for the treatment of . . . stomach ulcers. It was given a warning label that if taken while pregnant, it would induce a miscarriage.
Miso has the most interesting history. Feminists in Brazil in the late 1980s noticed the warning label. Given no legal access to abortion in Brazil, they started taking it and spreading the word that miso could be used as a safe and effective means of abortion. And it was something you could buy at any local pharmacy. This self-use then led to clinical trials, where it was legitimized and moved to clinical use.
In the decades since, miso has been used off-label for medication abortion, induce labor, prevent postpartum hemorrhage, and more. It’s really an amazing drug.
In fact, much of the world relies on miso-only abortions where mife is less accessible.
Why isn’t miso only routinely used in the U.S.?
Clinical consensus has held that the combined regimen (mife+miso) is more effective at ending a pregnancy than miso only. This is primarily based on pooled data across a wide range of studies that included a wide range of ways people can use the medication: i.e., different dosages, different routes of administration, and different intervals between doses.
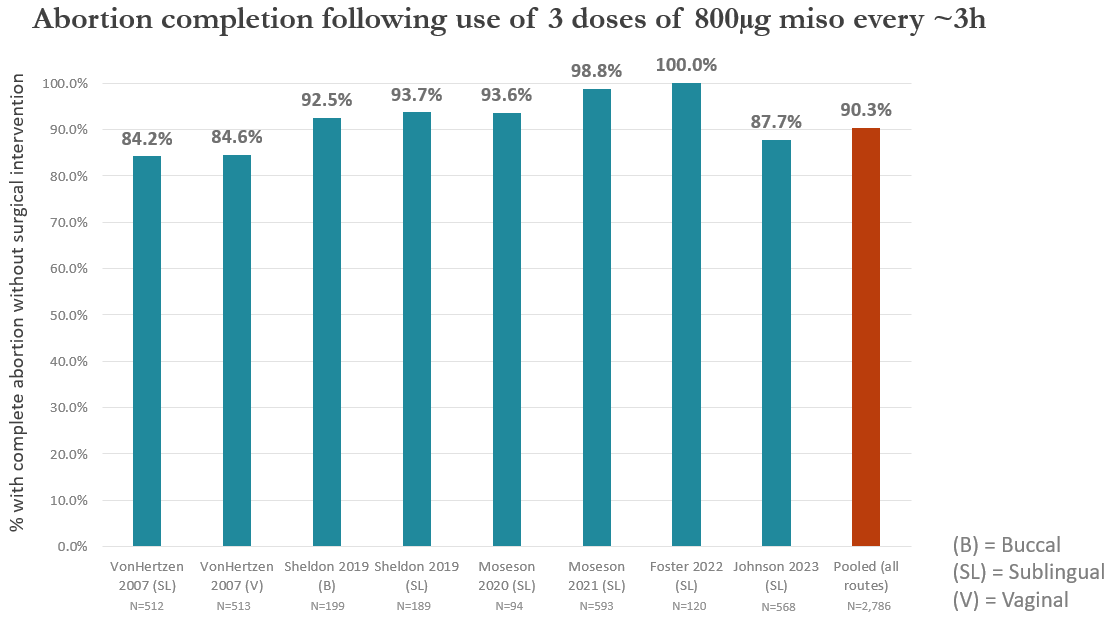
But if we look at the studies that report on a specific regimen (3+ doses of 800ug miso taken every three hours), miso only may be more effective than commonly thought. Across eight study groups that looked at 3+ doses of miso only, upwards of 90% had a complete abortion (compared to ~95% expected for the combined mife+miso regimen).
Updated graph from Dr. Heidi Moseson’s presentation in the Society of Family Planning webinar, “Misoprostol alone for medication abortion”, February 16, 2023
Miso only for abortion is also safe: only 0.7% of ~12,000 miso only users from a 2019 meta-analysis had a blood transfusion or were hospitalized for miso only abortion-related reasons.
Bottom line
As one journalist recently put it:
“It turns out our narrative has been backward. Biologically speaking, mife is the sidekick, and miso the superhero. Mife is the opening act while its counterpart carries the show.”
Restricting access to mife is epidemiologically baseless given 23-years of robust safety and effectiveness data. Yet, even with constrained choice, this does not mean that all medication abortion is off the table. People will still have access to a safe and effective method of medication abortion care: miso only. Let’s hope it doesn’t come to this.
Love,
YLE and HM
In case you missed previous posts:
Heidi Moseson, PhD, is a reproductive epidemiologist and scientist at Ibis Reproductive Health. She studies abortion access in the U.S. with a particular focus on self-managed abortion with medications.
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank and is a senior scientific consultant to a number of organizations, including the CDC. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below: