There are few better emblems of the failures of the US system of medical care than its inability to consistently provide insulin to Americans who need it.
The drug was discovered 100 years ago, and it provides essential and ongoing treatment for millions of people living with diabetes, one of the most common chronic diseases in the country. And yet one in six Americans with diabetes who use insulin say they ration their supply because of the cost. Some people end up spending nearly half of their disposable income on a medicine they must take to stay alive.
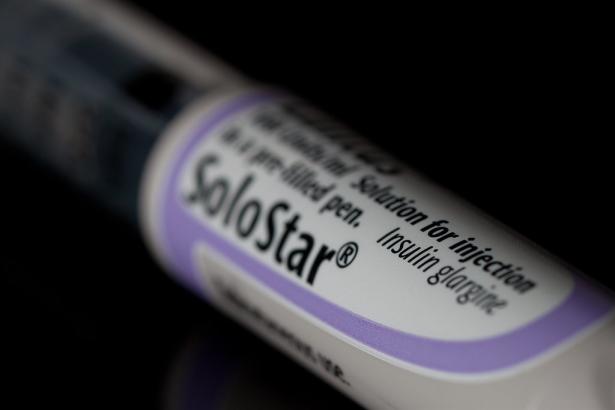
Though insulin generally costs less than $10 per dose to produce, some versions of the drug have a list price above $200. This is in part because, in the US, a warped market has allowed three companies to dominate the insulin business.
But if some states have their way, that may be about to change.
With California leading the way, a handful of states are considering trying to disrupt the market for essential medications, starting with insulin. The plan would be to manufacture and sell insulin themselves for a price that is roughly equivalent to the cost of production.
Their premise: Take away the private market’s profit motive and maybe states can deliver affordable insulin as a wholly public enterprise, run by civil workers, that does not need to make money. Because these states buy a lot of drugs too, through their Medicaid programs and the health plans for government workers, they would also reap the rewards if those drugs are cheaper.
“If we can drop the cost of insulin, we don’t have to make money on selling it. We get the savings as a purchaser,” said Anthony Wright, executive director of Health Access California, which has been a leading advocate of the public insulin plan and provided guidance to state legislators and Democratic Gov. Gavin Newsom’s office.
As his colleague Chris Noble, who has Type 1 diabetes, put it: “Just providing an actual at-cost alternative has the potential to really be disruptive for the pharmaceutical industry.”
States have become more ambitious in their policies for tackling the insulin affordability crisis because the scale of the problem continues to grow and the federal government seems capable of taking only limited action to address it. The price of some insulin had grown by 1,000 percent over the past 20 years, far outpacing inflation. And the number of Americans with diabetes is projected to grow to nearly 55 million by 2030, from the current figure of roughly 37 million.
Medicare, the federal health insurance program for seniors, is about to institute a $35 per month cap on insulin costs for its beneficiaries, a provision of the Inflation Reduction Act that Democrats passed last year. But, because of the Senate’s arcane rules, they could not establish the same cap for private insurance, which covers more than half of Americans.
A few states have passed their own out-of-pocket caps, but even a small cost burden, as little as $10, can discourage people from taking necessary medications. States have also sued the drug companies that currently produce insulin, asking the courts to intervene and stop the unfair market practices that they say inflate the drug’s price.
But those are half measures, chipping away at the high cost without fundamentally altering the market that has allowed a drug, which costs a few dollars to produce, to be sold at an enormous markup. A publicly produced insulin — a public option, you might call it — would be a consequential innovation. And if successful, it could open the door for more public projects to produce essential medications more cheaply than the private sector.
“I think there’s a window open now because federal action has been so limited,” Dana Brown, who has developed ideas for public pharmaceutical production in her work at the Democracy Collaborative, told me.
Why insulin is so stubbornly expensive
Insulin was discovered in 1921 by four men: Frederick Banting, James Collip, John Macleod, and Charles Best. They extracted the hormone insulin from the pancreas of a dog and gave it to another dog with diabetes, to see if it could control the second animal’s blood sugar as a substitute for the insulin it would normally make on its own. They then quickly tested the extract on a human, a young man who had Type 1 diabetes, and found that it was successful in managing blood sugar in a person too.
It was an enormous breakthrough: Before the discovery of insulin, people with Type 1 diabetes could expect to live less than three years. The inventors recognized the significance of their discovery and sold the patent for insulin to the University of Toronto for $1, with the hope of making it as easily available as possible.
“Insulin belongs to the world,” Banting reportedly said.
But those altruistic aspirations have been, over the years, eroded by private enterprise. Fledging for-profit drug companies recognized a business opportunity and quickly began developing their own insulin products. Longer-lasting insulins started coming on the market in the 1940s and ’50s.
Then in the 1980s, drug companies figured out how to mass-produce human insulin and then focused on developing artificial insulins that can be tweaked to make them act more quickly or last longer. As artificial insulins became the standard of care in the 1990s and 2000s, the three manufacturers that produced them gained more control over the US insulin market — and in the following decades, America’s insulin affordability crisis took off.
Most people don’t pay the list price for insulin, though depending on the kind of health insurance they have, patients can be on the hook for a lot of money. A 2017 study found that Americans with high-deductible insurance plans paid an average of $141 per month for their insulin. A young man in Minnesota with Type 1 diabetes, Alec Smith, died in 2017 because he could not afford the $1,300 out-of-pocket price for his prescription once he was dropped from his parents’ health insurance when he turned 26.
The newer artificial insulins can be very valuable for people with diabetes who need to time their insulin injections with meals in mind, though it is not clear that artificial insulin is more beneficial than bioengineered human insulins for some patients, such as those with Type 2 diabetes. But, according to many academic experts, the amount of innovation in the insulin business hardly justifies the current costs for insulin products. Insulin is still, at its core, more or less the same product that debuted a century ago.
Nevertheless, pharmaceutical companies stand to make a lot of money by continually refreshing their products. Thus, the three major insulin manufacturers in the US — Eli Lilly, Novo Nordisk, and Sanofi — continue to do that, and thereby maintain their control of the country’s insulin supply. The main mechanism the US has for bringing down prescription drug prices is allowing generic drugs to compete with brand-name versions. When a company develops a new drug, it gets a period of exclusivity, 10 years or more, in which it is the only one able to make or sell that drug. But after that exclusivity period has passed, other companies can make a carbon copy and sell it at a lower price. Studies find that once several generic competitors come on the market, prices drop significantly.
But pharma companies are savvy about finding ways to extend their monopolies, with insulin and other drugs, by making minor tweaks to the chemical compound and asking for a patent extension. In the case of insulin, the companies can also modify the delivery device to protect their market share. Each product is meant to be used with specific, company-designed injectors. Though the patents on the artificial insulin developed in the 1990s have started expiring, these companies continue to hold and extend monopolies on either their devices or other chemical compounds, making it harder for generic competitors to enter the market.
Other federal regulations have added to the challenge. The FDA began to treat insulin as a biologic drug in 2020 — meaning it is made with living materials instead of combining chemicals like conventional pharmaceuticals — which comes with a different set of standards for generic versions, which are known as biosimilars, as well as manufacturing challenges given the precise conditions these products must be made in. Biosimilars can cost up to $250 million to produce and take up to eight years to bring to the market, versus a one-year investment of as little as $1 million for conventional generics. And unless the FDA recognizes a new generic insulin as interchangeable with the products already on the market, health insurers might not want to cover it and doctors may not be willing to prescribe it.
To add one more layer of difficulty, the current manufacturers can always decide to drop their prices to crowd out new generic competitors, given the gap between the retail price and the $10 cost of production. The first biosimilar drugs have come onto the market in the past few years, but only one of them has been deemed interchangeable with the brand-name version; ultimately, in late 2021, it was priced at only $20 less than the brand-name insulin it was competing with. More competition is needed to meaningfully depress prices.
“We know why it’s happening and our government has failed to take action,” Hilary Koch, whose young son has Type 1 diabetes and who sat on Maine’s commission exploring the feasibility of the state producing its own insulin, said. “We know that there are thousands if not millions of dollars lost every year from people ending up in hospital or people having complications due to poor management of their diabetes. When we talk about improved management, that starts with access to insulin.”
Given their tight control of the market, insulin manufacturers could afford to lose a lot of their margin by cutting prices and still make a profit. That is a vulnerability that California, with its plan for the public production of insulin, is trying to exploit.
California’s plan to produce its own insulin
California’s program to produce a cheaper generic insulin has already cleared the first two critical steps: authority and funding. The state legislature passed a bill creating the authority for the state to produce its own insulin and it has appropriated $100 million to support the effort.
The state is taking a two-phase approach. In the short term, California has put out a request for proposals from existing enterprises that could produce generic insulin for the state as a subcontractor in the next few years in order to try to deliver relief as soon as possible.
One possibility would be Mark Cuban’s at-cost drug company, through which the NBA owner and venture capitalist has sought to provide cheaper medications directly to patients who pay out of pocket. Another is a relatively new nonprofit enterprise, Civica RX, which launched in 2018 as a collaboration between several hospital systems to produce cheap generic versions of essential medicines; its goal is to bring a generic insulin to the market by next year. California’s contract is expected to be announced in the coming weeks.
But in the long term, the plan is for a government factory operated by government workers producing government-owned medication. The state would have its own public production facilities, staffed by civil workers, which would sell generic insulin for the same cost needed to produce it, plus perhaps a small percentage to cover auxiliary costs for the program.
The $100 million in funding is split evenly between the short and long term. But that long-term vision will take time. Even if the state were to retrofit an existing factory for insulin production, that construction work could take years, as would hiring a workforce to oversee it. Once production is up and running, California would need to hit more targets — most importantly producing a product that the FDA says is interchangeable with existing insulin medications.
The Golden State is probably the best home for a project like this. Newsom has put a lot of political and literal capital behind it, and the state’s politics are such that Democrats are likely to remain in control for the foreseeable future. The generic insulin plan should have a long enough runway to see if it works.
If California really can produce its own generic insulin, then advocates in the state say it will be an almost can’t-lose proposition. Even if the private manufacturers were to drop their prices dramatically in response to a cheaper public option coming on the market, that is still a win for patients and for the state, which would save money on Medicaid and state employee insurance programs. There are international precedents for public drug production: Sweden adopted one in the 1970s and it continues to operate in a modified form in which the state is the only shareholder in companies that produce and sell drugs.
The one type of competition private insulin manufacturers have not had to face is a venture that doesn’t need to make a profit. I asked the current major insulin manufacturers what they thought about California’s initiative. They said they welcomed any competition and pointed to their own efforts to provide more-affordable insulin.
But the advocates working on the efforts in California think litigation or other efforts to slow them down could begin as the state gets closer to putting a product on pharmacy shelves.
The long-term vision for public pharmaceutical production
If manufacturing a cheap generic insulin proves viable for California, the consequences could be enormous and stretch far beyond insulin. California would provide proof of concept, and a fledging public marketplace for public pharmaceutical production could potentially emerge.
Advocates see an opportunity for state governments to disrupt the pharmaceutical industry. Let’s say California were to prove successful at developing its own generic insulin. Once it has the manufacturing capacity, it could sell that insulin to other states, helping lower the drug’s cost across the country.
Other states could develop and sell generic drugs of their own. Washington State and Maine are already following California’s lead, though they are not as far along. Washington has authorized, but not yet fully funded, the development of a program for the public manufacturing of generic drugs. Maine created a bipartisan commission to explore the possibilities, which is expected to deliver its final report to lawmakers soon. Lawmakers in Michigan have also expressed an interest in such a project.
If California succeeds, it’s possible that, eventually, a state like Washington or Maine would devote its efforts to a different essential and expensive medication. Other options could include drugs experiencing a shortage, drugs with expired patents but no generic competition, or high-priced medications with inequitable access such as EpiPens or asthma drugs, Brown said. States could then over time specialize in manufacturing specific medicines and trade with one another for other critical drugs.
This may sound far-fetched, but the public production of medicine is not entirely novel. Michigan used to produce its own vaccines through a state-run enterprise until the 1990s. Massachusetts still does, through the UMass college system, with the state providing funding to those institutions to produce vaccines, which are distributed to state residents at no cost.
Long-term trends toward privatization and the declining public trust in government’s ability to accomplish major projects, along with the mighty lobbying power of the drug industry, worked to discourage public officials from ideas as ambitious as the public production of a generic insulin. But the crisis of its costs has reached the point where states are compelled to intervene.
California’s experiment will be the most important test of that concept, and it will be years before we know whether it worked. But if it does, it could prove a pivotal moment in the effort to make essential medicines more affordable for Americans.
Dylan Scott covers health care for Vox. He has reported on health policy for more than 10 years, writing for Governing magazine, Talking Points Memo and STAT before joining Vox in 2017. TWITTER RSS
Millions turn to Vox to educate themselves, their family, and their friends about what’s happening in the world around them, and to learn about things that spark their curiosity. Financial contributions from our readers are a critical part of supporting our resource-intensive work and help us keep our journalism free for all. Please consider making a one-time contribution to Vox today.

Spread the word