Some of the most common infectious diseases are caused by bacteria. They range from minor skin infections to meningitis, TB and pneumonia.
Before the advent of antibiotics, about one in three Australians died before the age of 30. People routinely died of pneumonia. A skin infection could lead to the amputation of a limb or even death. More people died from bacterial infection than anything else on the planet.
Penicillin, the quintessential antibiotic, was discovered in 1926, and the golden age of antibiotic development followed the end of the Second World War. Dozens of antibiotics were discovered every year from the '50s through to the '70s, and they changed medicine. Common procedures like open-heart surgery, chemotherapy for cancer patients with depressed immune systems, organ transplants, even hip replacements would not be possible without antibiotics.
Professor Matt Cooper, director of the IMB Centre for Superbug Solutions at the University of Queensland, says that although many of the initial serendipitous discoveries were at universities, the vast majority of the compounds came from pharmaceutical companies.
'We all know Pfizer, which famously developed Viagra and Lipitor—blockbuster drugs. But actually Pfizer was an antibiotic company for the first 30 years of its existence,' he says.
'There were 30 or 40 pharmaceutical companies around then that were actively involved in developing these drugs, because they were quite valued by society and they were used a lot. They really did save millions and millions of lives.'
Antibiotics in agriculture and unintended consequences
In the '50s, the agriculture industry started to use antibiotics on livestock.
'Farmers and people with chickens, eggs, beef, seafood, realised they could get far more productive output from growing animals, particularly when you start to put lots of animals in a closed space,' says Cooper.
'It makes perfect sense, if you put lots of people in a crowded bus in winter you're more likely to get a cold. If you put lots of fish in the water close together in intensive agriculture, they are more likely to get infection. We started to use antibiotics in agriculture quite aggressively very soon after we started using it in man.'
Farmers also discovered that if you give antibiotics to a food stock animal every day, in general the yields are much higher—you will get a slightly heavier chicken or a slightly bigger fish.
Professor John Turnidge, who led an Australian government inquiry into the use of antibiotics in food-producing animals in the late '90s, says that the overuse of antibiotics—so-called growth promoters in agriculture—has had unintended consequences.
'They didn't quite recognise that using antibiotics in low doses over a long period of time is the most perfect storm for driving antibiotic resistance,' he says.
'Over a long time, in at least a good chunk of my working life, the industries involved have tried to deny that there was any link between that use and use in humans. They forgot a fundamental piece of biology—bacteria are everywhere, they're everywhere, and we all swim in the same gene pool.
'Genes will go from anywhere to anywhere, provided the bacteria move and have contact. So we can't isolate ourselves any more than the animals can isolate themselves from us.'
No new drugs to treat the superbugs
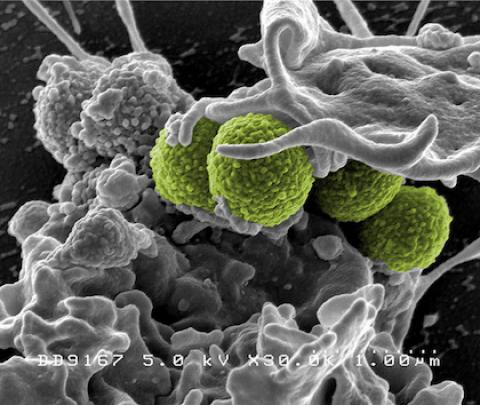
Along with the rise in antibiotic use came genetic mutations enabling bacteria to resist antibiotics—so-called superbugs. Turnidge says that means bacteria have evolved mechanisms that make them resistant to many of the most commonly-used antibiotics. And that means there may be only one or two options left to treat a given strain.
'In some cases, we have no options,' he says. 'Multi-drug resistance is resistance to lots of antibiotics; extreme drug resistance is something that is very, very rare but growing now in the world where we have no options left.
'When we first started using antibiotics they were seen as miracle drugs, and people really valued them, society valued them, they were precious compounds. We were blessed by our own innovative discoveries because we kept on finding new and better antibiotics every year.'
He says antibiotic use exploded around the world between the '70s and '80s, as more antibiotics came to market and became cheaper. But the more times a drug is used, the greater chance there is that the bug becomes a superbug.
'When we give antibiotics inappropriately, when we don't finish the course or we take them when we've got a virus infection—because antibiotics will not work if you have a virus infection, and many common colds are viruses—we are just encouraging resistance to rise.
'So we've now got to the stage where we just treat them as a commodity. We've always thought scientists will come up with a new drug; we don't have to worry about it. That's not happening anymore. We getting to the stage where there are no new drugs to treat the superbugs.'
A broken market
Given pharmaceutical companies were so successful developing antibiotics during the second half of the 20th century, why haven't they managed to get on top of antibiotic-resistant bacteria?
Professor Kevin Outterson, from the Boston University School of Law, says that the global antibiotic market is broken. They're not like most drugs, which you want to sell as much as possible of as soon as you bring them to market.
'If you had a new heart disease medication or something for depression that worked better, we'd want everyone to be using that new drug. For antibiotics it's almost the opposite,' he says.
'When you have a new drug, it's almost the last thing that the doctor or the hospital wants to use. We want to save that, for really good reasons, for the worst cases. We want to save it for the future and use the generic if we can or the antibiotic that's currently in use now that's still effective.'
From the drug companies' perspective, Outterson says, it's as if they have been told not to sell their new product: 'Imagine that you are Apple and you had to prove that all the iPhone 4s and 5s and 6s were completely worthless before you could sell your new model. It just makes the business really difficult.'
Moreover, unlike drugs for high blood pressure, diabetes or depression, antibiotics are generally taken in short courses. Many of the antibiotic-resistant strains of bacteria infect thousands, rather than millions, of patients, further eroding the business model for new antibiotic development.
'For example, in the United States there is an infection called CRE; it's one of the three superbugs that the US Centres for Disease Control is concerned about,' says Outterson.
'It would be wonderful if we had a drug that targeted that condition ... but there's only about 9,000 patients a year who have this infection in US hospitals, and most of those can be treated by another drug.
'So are you going to make a drug that you might only sell a couple of hundred doses of in a country like the United States per year? It's difficult to do that unless you know you are going to make an awful lot of money per dose.'
Antibiotic development expertise disappearing
Matt Cooper says there are now few researchers left—less than 1,500, he estimates—who know how to discover and develop antibiotics.
'AstraZeneca just downsized from hundreds of people down to 14,' he says. 'Cubist was bought out by Merck, a very large pharmaceutical company. They fired all 120 antibiotic researchers. Every year we are seeing hundreds of people leave the field.
'All that knowledge, all that experience about how to discover and develop these wonderful drugs is disappearing as we speak.'
Cooper says the root of the problem is the market-driven nature of the pharmaceutical industry; companies make more money by making expensive drugs and selling a lot of them.
'We can't force pharma to go into an unprofitable area,' he says. 'They are just not going to do it. They are companies that are required to make a profit by their shareholders.
'What we can do is think about different models. The societal value of antibiotics is huge. I can talk about lots of examples where a superbug infection in a hospital has shut down a ward or in some cases shut down a hospital. It's a huge impact on costs and lives and society.
'So let's think about an insurance premium. If you develop a new antibiotic that kills these MDR superbugs, you get paid $100 million a year. It doesn't mean we have to use the drug, we can keep it for those special cases where we can really save lives, but I think we have to think more creatively about the economics of this development, and we need to do it soon.'
Breaking the habit of unnecessary antibiotic use
Outterson says we need to be much more aggressive in protecting and conserving the antibiotics we already have by reducing their unnecessary use in medicine and in agriculture.
'We also have to be careful about the people around the world right now who are dying because they lack access to antibiotics,' he says.
'Right now, according to an article that our group published in the Lancet earlier this year, more than 450,000 children under the age of five die each year from a susceptible bacteria. In other words, they could be saved with amoxicillin, a generic, cheap antibiotic that we know works.'
'We need to do all these things simultaneously: push the drugs out to the people that need them, get them out of the bodies of the people who don't need them, be sensible about what we are doing in agriculture, and simultaneously create a few new ones for the future.'
Turnidge emphasises the need for Australians to use antibiotics more responsibly. 'We've become overly dependent on them,' he says.
'The data in Australia suggests that the amount we consume is at least double the world class standard, which is held by the Netherlands. We use twice as many antibiotics and we are not twice as sick.
'Antibiotics have become part of our culture, and we've got to break that apart and minimise our antibiotic use to the point where we save it for those people who really need it, like those with meningitis or septicaemia.'
[Keri Phillips presents and produces the Australian Broadcasting Corporation's Radio National (RN) Rear Vision program together with Annabelle Quince.]

Spread the word