The U.S. Department of Health and Human Services announced on Tuesday that it will cancel $500 million worth of projects dedicated to designing messenger RNA (mRNA) vaccines for pandemic preparedness.
The move drew sharp criticism from medical and health experts. “Scrapping the fastest platform we have is a reckless move rooted in a fundamental misunderstanding of vaccinology,” wrote Jake Scott, an infectious diseases specialist and clinical associate professor of medicine at Stanford University, on the social media site Bluesky.
The use of mRNA in vaccines has opened new doors beyond infectious disease. Researchers are investigating promising mRNA vaccines for pancreatic cancer, which currently has a five-year survival rate of just 13 percent. They’re also studying mRNA treatments for multiple other types of cancer, autoimmune disorders and genetic diseases such as sickle cell anemia.
What makes mRNA so valuable is its programmability—and, for pandemics, the speed at which it can be programmed.
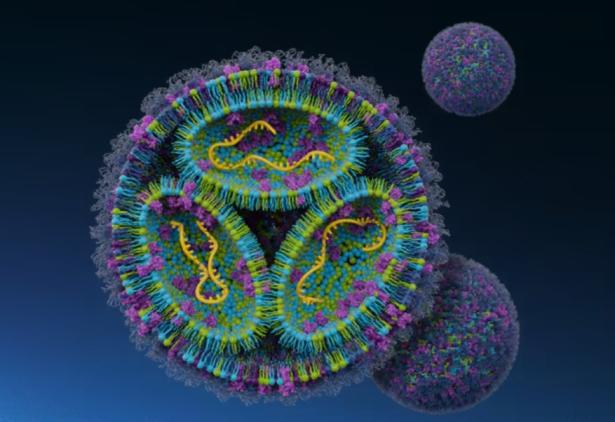
Traditional vaccines introduce an inactivated or dead pathogen into the body so that the immune system can learn to recognize and fight it: the immune system stores that memory in case it should ever run across the real thing. Vaccines that use mRNA, on the other hand, instruct the body’s own cells to make parts of a protein in or on a pathogen. The body will then learn to recognize this protein without having to fight off the full infectious agent.
These vaccines do not interfere with cellular DNA, which is the permanent blueprint, tucked away in the cell nucleus, that tells the cell’s machinery what proteins to make. Those proteins, considered the cells’ workhorses, then carry out various and critical functions throughout the body. Messenger RNA is a middle step in the process: DNA produces this single-stranded RNA, which then tells the cell how to assemble amino acids into proteins. The mRNA instructions from vaccination degrade within a few days, and studies suggest the spike protein generated by such vaccination against COVID lasts about a month in the body.
When making a traditional vaccine, researchers have to manufacture the antigens, or proteins that stimulate the immune system. They might do this by growing a whole virus in bacteria or chicken eggs and then weakening or killing the pathogen with heat or chemicals. In other cases, they use organisms such as yeast that are genetically engineered to churn out pieces of a virus that are familiar to the immune system. In these cases, the manufacturing process takes time, testing and tweaking. For mRNA vaccines, developers design the genetic instructions for an antigen on a computer. The manufacturing process remains the same from vaccine to vaccine, with only the genetic instructions changing. This allows researchers to develop multiple vaccines at once, as well as to develop vaccines that contain mRNA to make multiple antigens for different infections.

Spread the word