There is a saying among epidemiologists: “If you’ve seen one pandemic, you’ve seen one pandemic.” Echoing this trade wisdom in an interview two weeks ago, Bruce Aylward, the assistant director of the World Health Organization (WHO), pointed out that each new pandemic follows its own logic, and those who rely on past experiences to draw conclusions for public health will make mistakes. With each new pandemic it is tempting to scour history books for parallels and lessons learned. But as many have stressed, the wisdom to be gained is often greatly exaggerated.
Still, it is possible to steer a course between the Scylla of historical blindness and the Charybdis of hasty generalization. In her book about the era of the Black Death of 1348, A Distant Mirror (1978), the historian Barbara Tuchman confines her remarks on the present to a few oblique lines in the preface. “If one insists upon a lesson from history,” she writes, it is, as the French medievalist Edouard Perroy contended, that “Certain ways of behavior, certain reactions against fate, throw mutual light upon each other.” My working premise is that although the pathogen may be new, the logic of social response is not, and it is here that we can see historical continuities. An especially telling case study—still an object of fascination and controversy among historians of health and disease—is the devastating outbreak of cholera in Hamburg at the end of the nineteenth century, the subject of Richard Evans’s superbly researched book, Death in Hamburg (1987).
On the morning of August 24, 1892, Robert Koch arrived at Hamburg railway station from his laboratory in Berlin. Germany’s most famous medical scientist, he was already credited with discovering the anthrax disease cycle and the bacillus that causes tuberculosis. In the 1880s he had traveled to Egypt and India, where he succeeded in isolating the bacterium responsible for cholera, and on his return to Berlin he was fêted by Kaiser Wilhelm, invested with the Order of the Crown, and put in charge of protecting the empire from epidemics of infectious diseases.
Nine days before Koch’s train arrived in Hamburg, a doctor in the neighboring town of Altona had been called to see a stricken construction worker, whose job included inspecting the sewage works. He was suffering from acute vomiting and diarrhea; the diagnosis was cholera. In the first sign of the lethal controversy that was just beginning to erupt, the physician’s superior medical officer refused to accept the diagnosis. From August 16 to 23 the daily count of cases grew exponentially to more than 300; over the following six weeks some 8,600 residents of Hamburg perished. Like a forest fire racing through dry tinder, the epidemic burned itself out in October, an ending helped by the efforts of Koch and his team.
As we know now, those deaths were totally preventable. The immediate cause of death was vibrio cholerae, but the city authorities were accomplices to mass mortality, having long resisted spending public money on public health and fearing that a declaration of cholera—with the quarantine and isolation sure to follow—would bring their trading city to a halt. In Altona, just outside Hamburg’s jurisdiction, there were few infections; in Hamburg’s sister port of Bremen, a self-administering former Hanseatic League city-state, there were just six cases, half of them recent arrivals from Hamburg. Hamburg suffered alone that year.
In their pitch and consequence these events have the narrative structure and moral tensions of a theatrical tragedy. Besides the cholera vibrio itself, which takes the shape of a comma (like its typographical counterpart, potentially catastrophic if inserted at a crucial juncture), the dramatis personae are Koch, the chemist and hygienist Max von Pettenkofer, the physician-anthropologist Rudolf Virchow, and a chorus of the afflicted themselves and some of their revolutionary spokesmen. There are five subplots. Science contends with superstition and fatalism; the new germ theory of disease disputes with so-called ecological or local conjunctural theories; militarized centralizing bureaucracy spars with liberal capitalism; the anthropocentric “epidemic narrative” that promises a return to the safety of life-as-normal wrestles with the logic of evolution operating on different timescales, from the microscopic to the macro-ecological; and last, an open, democratic society questions its limits.
As we will see, some that is old is new again.
Cholera: the nineteeenth century’s most fearsome pandemic
Until the early nineteenth century, cholera was endemic to the Ganges Delta in Bengal, but it appears not to have been found elsewhere. The causative bacillus lives in warm water and multiplies in the human intestine, transmitted by fecal contamination. That was cholera’s macro-ecology: all it needed was to survive in just a few shallow wells during each dry season, with every annual flood spreading the germ far and wide.
Along with the great famine of the 1770s, one of the lethal gifts of the English East India Company was opening up routes whereby cholera could spread far more widely, colonizing new places as a kind of biological blowback. British investment in widespread irrigation to grow cotton created the perfect ecology in which the vibrio could find multiple local reserves—irrigation ditches and canals, reservoirs, wells, water tanks—and become endemic. In 1854, the English physician John Snow elegantly demonstrated that the infection was water borne. He showed this through an epidemiological study still heralded in textbooks today: after painstakingly plotting cases on a London street map, he asked each affected household where they obtained their drinking water, tracing the source to a single contaminated pump on Bow Street.
According to legend, Snow asked the local alderman to remove the handle on the pump, and new cases promptly ceased. In fact, as Snow himself admitted, the epidemic was already subsiding by that time, but he had made his point: the dominant “miasma” explanation—that the disease was caused by locally-generated impure air—had a competitor theory that had the virtues of being simple and provable. In the same year that Snow was mapping the outbreak, the Florentine microbiologist Filippo Pacini described the bacillus, which he had extracted from the autopsies of victims. But Pacini had no powerful political apparatus behind him to endorse and broadcast his breakthrough, and medical studies were not sufficiently systematic for the correct conclusion to be drawn. Thus the paradigm shift was not automatic. Rather, advocates of the miasma theory refined their arguments, contending that complicated local interactions of soil, air, and personal characteristics accounted for the vagaries of the disease. Prominent among the exponents of these views was the indefatigable chemist, hygienist, and health reformer, Max von Pettenhofer, whom we shall encounter in Hamburg shortly.
Cholera first reached Europe in 1830, causing mass mortality, panic, and unrest. The vibrio produces particularly nasty symptoms in its human host: once it enters the intestine, its ideal micro-ecology, it multiplies exponentially and drives out the resident microbiota within just a few hours. The stricken body loses control of its functions, lapses into fits of uncontrollable vomiting, diarrhea, and muscle spasms, and turns blue and bloated. Catastrophic dehydration then causes death in about half of those infected.
For the emergent bourgeoisie in Europe, the manner of cholera’s attack was no less terrifying than the prospect of mortality: an individual could be stricken at dinner, or in a tramcar, causing revulsion and terror among his or her companions. Just as disturbing to the authorities were “cholera riots” in which peasants and the inhabitants of the newly expanding, grossly unsanitary industrial cities attacked landlords, city authorities, and in some cases physicians, accusing them of using the disease as a pretext for driving them out of their homes and seizing their property. Sometimes the poor even blamed the rich for having introduced the disease for that very purpose.
Subsequent cholera pandemics coincided with the 1848 uprisings throughout Europe—with localized outbreaks for a decade, including the one that prompted Snow’s investigation—and the wars of the 1870s. In 1891 famine struck Russia, prompting a wave of westward migration by hundreds of thousands of people one or two economic steps up from the starving peasantry, and the vibrio traveled with them. Those tired, poor, huddled masses dreamed of America, and the Hamburg-America shipping company was the most-traveled route to the New World. The German health authorities registered the cases as the migrants moved; many were stopped at the border, but some passed through undetected. The epidemic warning lights were blinking red.
Medical and ecological controversies, then and now
Cholera is a pantomime villain in this drama: stealthy, sudden, and lethal. At the time of the Hamburg epidemic, there was still much controversy about its etiology. Was it a contaminant invader? Did it emerge when there was a special configuration of local conditions? Thirty years after Snow and Pacini, and eight years after Koch isolated the vibrio, there still wasn’t medical unanimity. Hamburg was to change that.
Scientific method was itself developing alongside medical discoveries, and Koch was in the vanguard of both. “Koch’s postulates,” as we now call them, were criteria for determining whether the agent of a disease had indeed been correctly identified. According to the postulates, the microbiologist had first to identify the suspected microbe in all infected individuals; then it should be grown in culture; thirdly he had to use the microbe to infect an experimental experiment and observe it sicken with similar symptoms; and finally isolate the same microbe in the sick or deceased animal. The experiment had to be repeatable. Ironically, Koch’s identification of the cholera vibrio did not fulfill his own criteria; despite his best efforts he could not induce cholera in an animal host. It only affects humans. There were also plenty of who, why, and where questions left unanswered about outbreaks—enough material for skeptics to make the case that the germ theory was, at minimum, incomplete.
The cholera controversies of the 1880s and 1890s were, nonetheless, the first conducted under the dawning light of the new microbiology. So-called “anti-contagionists” and “localists” argued that there surely had to be other conducive factors such as the weather, the soil, or the temperament of the individual patient. Radicals asked, why was it that the proletariat were always hardest hit? (Studies of disease patterns show that this wasn’t always the case, but it was true often enough to serve as grist for social reform agendas.)
In the case of the COVID-19 coronavirus today, the mysteries are fewer, the scientific method is more robust, and the speed with which controversies are resolved is many times faster. The lapse between identifying a new disease and knowing its pathogen is closer to five days than five decades. The coronavirus was isolated within a few days of the first cases and its entire genome was sequenced and available online two weeks later. We have the benefits of testing and tracing and massive computational power in charting epidemiological scenarios. Still, much remains uncertain, and epidemiologists continue to revise their understanding of the case fatality rate and vulnerability factors. We do not know whether COVID-19 will infect 20 percent, 40 percent or 70 percent of the population. It is important to parse our ignorance, separating out what risk is calculable now, what risk will be calculated when we have better data, and what is profoundly uncertain because it cannot be captured by data gathering.
Consider an example. In their influential modeling of possible trajectories and the impact of “non-pharmacological interventions” (NPIs, by which they mean policies such as quarantine or social distancing), Neil Fergusson and colleagues at Imperial College London include the following caveats:
It is important to note at the outset that given SARS-CoV-2 is a newly emergent virus, much remains to be understood about its transmission. In addition, the impact of many of the NPIs detailed here depends critically on how people respond to their introduction, which is highly likely to vary between countries and even communities. Last, it is highly likely that there would be significant spontaneous changes in population behaviour even in the absence of government-mandated interventions.
There are two caveats here, and they should be treated differently. The first is that the basic data for sound epidemiology are not yet known, but better approximations are constantly becoming available. This is an exercise in better calculation of risk. The second caveat, which Fergusson divides into two, is that outcomes will depend upon how people respond, both to official policies and because of other changing beliefs. Health behavior is harder to measure than epidemiological constants. The point is that the social component of the trajectory of the epidemic is uncertain in a way the medical component is not: although the margins can be narrowed, the risk really cannot be quantified. In a series of blog posts examining the intersection of health, environment, and politics, the scholar of science and technology policy Andy Stirling explains, “the crucial distinction between ‘uncertainty’ and ‘risk.’ A risk is what results from a structured calculation that must necessarily reflect a particular view. An ‘uncertainty’ is what these risk calculations might leave out.” Health behavior is just one part of this.
Another element of uncertainty is that epidemics are inflection points in evolution across different scales, from the microbial to the planetary. Pathogens evolve; microbes populate the microbiomes of animals and plants, the soil and the water; remnants of viruses are found in our DNA. For bacteria and viruses, the boundaries of the human self hold no meaning, and the more that we discover about the viral remnants in our DNA and the richness of our microbiomes, the more we are compelled to acknowledge that point of view. The vicious nineteenth-century strains of cholera retained their prior strategy of rapidity and lethality, killing about half of the humans they colonized. In the mid-twentieth century, the “El Tor” strain evolved a new strategy of lower virulence. This is a common adaptive trajectory for pathogens, which prosper by treating their hosts as symbiotes instead of wantonly destroying them. The first pandemic of any new pathogen is, for the human population, usually the worst—so it was for bubonic plague in Asia and Europe, smallpox and measles in the Americas, and cholera. It is no solace to Homo sapiens facing COVID-19 today.
Ecosystems change too. Most of the new pathogens that infect humans are zoonotic: they jump the species barrier, from wild monkeys or bats, or from domesticated chickens or pigs. This has always been the case. But in the past, a zoonotic pathogen might infect a band of hunter-gatherers; today, thanks to a globalized, deeply interconnected world, a single local outbreak can become a pandemic in a few weeks. Another new factor is the proximity of humans to domestic animals and factory farms. The 90 percent of nonhuman terrestrial vertebrate biomass on the planet that is husbanded for our consumption lives—if we can call it living—in ecosystems such as feedlots that have no precedent.
As Mike Davis observes in The Monster at Our Door: The Global Threat of Avian Flu (2005), these are perfect incubators for new zoonoses, especially for avian influenza, which can evolve first in chickens, then jump to pig populations that act as a kind of pathogenic evolutionary accelerator, and finally make the leap to humans. In turn, each new human-pathogen dyad alters the ecology of global public health and disease: our built environment changes (in the nineteenth century with the introduction of municipal water supplies, for example); our biochemical environment changes (supplementing animal feed with antibiotics, for example); and our health behaviors change. Meanwhile, climate change is altering the ecologies of infectious diseases in ways that we cannot predict. The post-pandemic world is a changed ecosystem.
Though a great deal of headway has been made into the study of these complex environmental factors, the uncertainties they introduce are left out of epidemiological models narrowly focused on predicting numbers of cases and deaths. The standard “epidemic narrative” consists of a stable “normality” threatened by the intrusion of a novel, alien pathogenic threat, followed by an epidemic and an epidemic response (of variable proficiency) and ends with a return to the status quo ante. That neat storyline simply doesn’t hold. In turn, in Hamburg 140 years ago and across the world today, what is “left out” depends on where you stand.
How liberals failed to prevent epidemics
So much for the microbial protagonist. Let’s turn now to the three human characters in our retelling of the Hamburg tragedy.
First on stage is the dominating and ultimately tragic figure of Max von Pettenkofer (1818–1901)—almost unknown today, but 130 years ago at the height of his professional fame and Germany’s most eminent chemist. He championed medical research, advocated clean air and urban sanitation, and mentored dozens of students. In the comic-book version of our Hamburg story, though, all these achievements count for naught: he is instead the villain whose obstinate pride failed the people of Hamburg twice over. His biggest shortcoming was failing to prepare for waterborne diseases and refusing to order the construction of filtration plants to treat the city’s drinking water supply, so that people were drinking water piped straight from the river Elbe to storage tanks and from there to their homes. As water levels dropped in the dry, hot summer of 1892, contaminants were washed downstream from riverside towns and from the barges that plied the waterway. Filtering through sand efficiently removes vibrio cholerae. Other cities did it; Hamburg didn’t.
Why did he take this stand? Despite the centralizing ambitions of the Prussian state, and the uniform color of its territories on the political map of Europe, the administration of Germany was not yet unified. Hamburg, the second-largest city and its richest port, still retained the legacy of self-government from its membership of the Hanseatic League. The city was run by its own senate and zealously guarded its powers to make independent policy decisions, especially in matters of trade. Indeed Hamburg was the most “English” city in Germany, governed by an assembly of its citizens—by its constitution, a small and privileged group of property owners; by its social history, an oligarchy of traders and lawyers. They disliked and distrusted the military-bureaucratic Prussian ways of state.
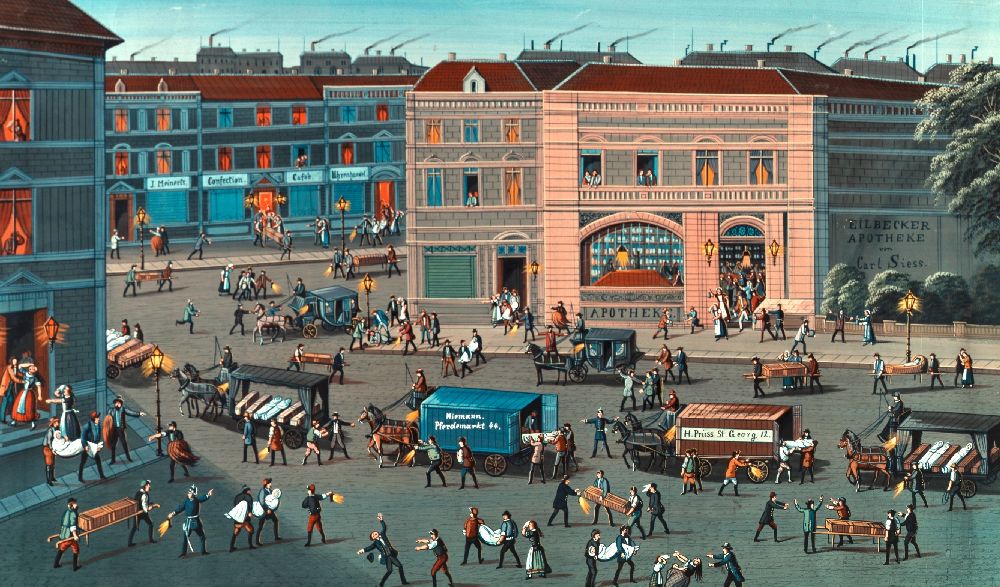
Detail from Cholera in Hamburg by Jean Speth. Image: Wikimedia Commons
Those citizens believed in small government, balancing the books, and individual responsibility for health and well-being. Spending their tax money on a filtration plant looked to be an extravagance that threatened both the fiscal health of the city-state and the ethic by which it had prospered. These laissez faire doctrines resembled those that had led Britain to the utmost parsimony in famine relief in Ireland and India—its colonial administrators holding fast to the belief that public debt was a more egregious sin than mass starvation, and that the hungry could only remedy their plight through learning the self-discipline of hard work and husbanding scarce resources.
The next-biggest failing of von Pettenkofer and his loyal disciples in Hamburg’s medical office was their refusal to accept the cholera diagnoses and issue a cholera declaration during those crucial days in August when the rate of infection was doubling each day. As we have now learned once again, to our collective cost, bacilli and viruses can multiply at an exponential rate. The delay of a day can make the difference between containing an outbreak and facing an epidemic.
Why did he not do this? Part of the explanation is the intellectual inflexibility of the man of high standing. The other part is material interest. Port that it is, in the 1890s Hamburg’s economy, and the prosperity of its plutocrats, depended on keeping the harbor open and the ships moving. Goods were coming in from England and the United States. The larger part of Germany’s exports were arriving by barge and train to be loaded onto ships destined for every continent, and the Hamburg-America line had regular sailings for New York, the decks packed with migrants seeking a better life on the far shore of the Atlantic.
If we read von Pettenkofer’s calculation as a straightforward tradeoff between profit and human life, we do him an injustice. Most of the public health measures to deal with cholera began as hand-me-downs from the medieval plagues, revised during the previous sixty years during the visitations of cholera, adapted each time based on a rule-of-thumb empirical assessment of what had worked and what hadn’t. New viruses and bacilli had emerged; society’s responses stayed much the same.
The first draft of the plague control playbook was drawn up in Italian city-states in the years after the apocalyptic shock of the 1348 Black Death. Much like cholera half a millennium later, the plague arrived explosively and killed in a gruesome and rapid way. Its mortality was extraordinarily high: overall, perhaps a third of the population of Asia and Europe succumbed, and in most European cities, half of the residents perished, sometimes in just a few weeks.
The calamity was widely attributed to divine wrath, to astronomical alignments, to witchcraft and sorcery. Italian princes, city elders, and merchants were more empirical. The first boards of health were set up in Venice and Florence in the same year that the plague appeared; these evolved into permanent magistracies over the next century, with authority to restrict travel and trade, and isolate infected individuals. Isolation hospitals, called lazzaretti, were set up to prevent contagion. Italian cities also issued certificates of health to important traders and diplomats, so that they could pass freely through checkpoints. The first passports were health cards.
Observing that the plague tended to appear first on ships from the east and then spread when those ships arrived in port, they began comparing notes and drawing up advice. Quarantine was first trialed in the Venetian port of Ragusa (now Dubrovnik) in 1377—its name refers to the forty days that suspected vessels were kept offshore to see if sailors and passengers fell sick. Within a few decades, the fundamentals of plague control had been worked out by trial and error: alongside quarantine, what we would now call notification of cases of infection, isolation of the sick, imposition of cordons sanitaires and travel restrictions, and disinfection (usually through burning the property of those infected). The main item missing from the list was carrier control: the role of rats—to be precise, rat fleas—as the reservoir of infection was not known, and systematic suppression of rat infestations was never contemplated, and presumably would have been considered impractical if it had been. Instead, people assumed that plague spread by human-to-human contagion.
The tools of plague containment were part of the scaffolding of the earliest administrative apparatus of the modern European state, and notably so in northern Italy. The science was somewhere between wrong and inexact, the motives mixed, the implementation quite often haphazard. Little wonder that critics condemned these measures as expensive, ineffective, and dangerous. The financial costs hardly need to be restated: the bureaucrats had to be paid, and interruptions to trade caused mercantile bankruptcies. Effectiveness could be questioned: the plague often managed to get through the defenses, and people would find ways of evading the restrictions or overwhelming the policemen dispatched to enforce them. The danger lay in the social unrest that followed unemployment, high food prices, and the intrusions of the police.

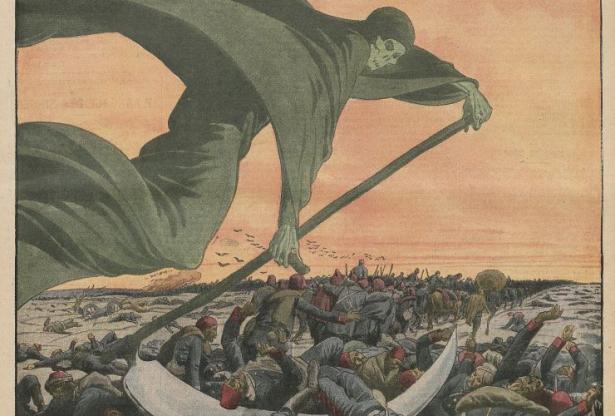
The Triumph of Death (c. 1562) by Pieter Bruegel the Elder. Image: Wikipedia
It wasn’t until 1894 that the pathogen was identified, simultaneously by Alexandre Yersin (a former laboratory assistant at the Pasteur Institute in Paris) and the Japanese biochemist Shabasaburo Kitasato (who had trained under Koch in Berlin). They both isolated the microbial cause, a pathogen carried by rat fleas, called Pasteurella pestis or Yersinia pestis—a victory for European science over Asian, and for France over Germany. Plague remained endemic in India and China at that time with sporadic outbreaks, but had vanished from Europe (the last epidemic occurred in Marseille in 1720). Exactly why plague disappeared from Europe remains one of the enduring mysteries of microbial history: was it changes in the rat population, in the ecology of the transmission zones on the eastern borderlands of the continent, or the effectiveness of Europe’s quarantines and lazzaretti?
The best-documented cases of the plague response toolkit are naturally the most recent, and a good (or bad) example was Bombay in 1896, which is germane to the Hamburg drama for two reasons. First, it illustrates the standard epidemic containment policies as deployed in the same decade. Second, it occurred two years after the Yersin/Kitasato breakthrough had revealed that the main mode of transmission was fleas-to-human rather than human-to-human.
Despite the scientific discovery, British officers of the Indian Civil Service remained convinced that the plague endured due chiefly to Indian backwardness. The historian Rajnarayan Chandavarkar observes that even though the medical and scientific experts were up-to-date on the most recent discoveries, their “policies, formulated on the assumption that the plague was a virulently infectious disease, proved at best oppressive and at worst fatal.” Among these, “stringent inspections” on the railroads turned up few cases, while “pumping the sewers with disinfectants” simply drove rats and the fleas they carried into houses, where they promptly spread the infection. The disorderly, distrustful, and sometimes violent response of the Bombay residents, dismissed as superstition by colonial officers, is perfectly understandable. The official cure—if indeed it can be counted as such—was arguably as bad as the disease.
Bombay also shows that von Pettenkofer was not alone in disputing the latest medical claims. Indeed, Hamburg was following well-established British precedent in downplaying the modes of transmission of pathogens, when commerce was at stake. After the opening of the Suez Canal in 1869, the International Cholera Control Commission in Istanbul insisted that British ships with infected sailors or passengers be kept at sea for the requisite forty days, bringing the (French-led) commission into conflict with ministers in London who insisted that quarantine regulations were a gross violation of the 1846 Free Trade Act. Influential English doctors insisted that the germ theory of cholera was “a humbug got up for the restriction of our commerce.” Until March 2020 at least, British public health policy retained a laissez faire strand quite distinct from continental Europe.
Von Pettenkofer’s doctrines are thus much more comprehensible in the context of these centuries of practice in epidemic control with limited outcomes, the oppressive aspects of quarantine and isolation, and the uncertainties of the medical science and epidemiology of the time. His medical and social beliefs were an odd mélange; he is hard to place in today’s political spectrum. He advocated “localism,” believing in particular that cholera became virulent only in particular kinds of soil, and that it needed a human body with the requisite moral and psychological preconditions to develop into the full-blown disease. He held that health was a matter for individual family responsibility, not state diktat.
In our drama, von Pettenkofer’s first fatal error began as a relatively minor fault, amplified by his inflexibility. He steadfastly refused to purify Hamburg’s drinking water supply by the relatively straightforward method of filtering it through sand, which efficiently removes the cholera vibrio. He could readily have accommodated the cleansing powers of sand into his general promotion of cleanliness and his view that the bacillus also needed a receptive soil to become potentially lethal. But almost as if gripped by a death wish, von Pettenkofer took a stand that water filtration was a needless expense without benefit. In our drama, we can imagine the audience silently urging him, “just filter the water supply! Just do it!”
His second disastrous error was his refusal to declare epidemic cholera on August 18, 1892, or over the following few days. Only on August 23, the day before Koch arrived, did the Hamburg medical authorities admit that the disease was present in their city. By that time every part of the city was affected.
The denouement of von Pettenkofer’s role occurs when he has been driven out of his post, but still rancorously defends his “local configuration” theory. He lays down the ultimate challenge to Koch: he will drink a solution containing the cholera vibrio and see what happens. The old man did this on October 7, 1892, recording the grotesque symptoms in his diary. He recovered, concluding that his view was vindicated: cholera needed both an infectious agent and also a conducive host. An identical experiment was undertaken by his disciple Rudolf Emmerich ten days later, which he performed on a stage in front of an audience of over a hundred people. Emmerich also survived. (Evans, in Death in Hamburg, suggests that Koch’s laboratory assistants, who provided the samples, suspected the purpose of the request and mercifully diluted the solutions.) Von Pettenkofer finally fulfilled his death wish with a pistol to his temple in 1901.
How the centralizers—and their science—prevailed
The Hamburg epidemic occurred at the inflection point in the rise of scientific medicine. The protagonist of this paradigm shift, the hero of the tale, is Koch (1843–1910): he is the one remembered for having taken charge of Hamburg’s failing public health system and clearing out the charlatans. When Koch arrived on the train from Berlin on the morning of August 24, carrying the Kaiser’s writ, he already knew the diagnosis was cholera; a doctor from Altona had arrived at his laboratory a few days earlier with a sealed jar containing samples from patients. But he apparently had no idea of how rapidly the disease had taken hold nor how negligent was the municipal response.
There was no official delegation at the railway station to meet the Empire’s highest-ranking scientist. Koch had to make his own plans: his first stop was the city medical office, where he arrived at 9 a.m. The chief medical officer was Dr. Johann Kraus, a faithful acolyte of von Pettenkofer: he turned up only thirty minutes later, and had little information to impart, for he had done nothing other than sneer at the “hyperactive behavior” of his counterparts in other towns (such as Altona). Koch’s next stop was the New General Hospital in Eppendorf, where the director, Dr. Theodor Rumpf, was ready to greet him at the door. Koch asked straightaway if there were cholera cases to report, and Rumpf promptly gave him the figures, whereupon Koch remarked to his companion, “The first man in Hamburg who’s telling us the truth!”
After visiting the hospitals, disinfection centers, and barracks where the migrants from Russia were housed awaiting their ships, Koch toured the old, overcrowded, ramshackle “Alley Quarters” in the city center. By this time he was becoming aware that hundreds were already dead. “I felt as if I was walking across a battlefield,” he said. And amid these unsanitary streets, courtyards, and canals, he was shocked: “In no other city have I come across such unhealthy dwellings, such plague spots, such breeding places of infection.” This was a man who had scoured the Alexandria and Calcutta hospitals in his search for the bacterial culprit. In the alleys he made a remark that became an infamous condemnation of Germany’s most cosmopolitan city: “Gentlemen,” he said, “I forget that I am in Europe.”
If any moment in our drama were to mark the shift in the paradigm for understanding epidemic disease, this would be it. This is the point at which the naysayers’ defenses became hollow, that the unresolved medical and epidemiological controversies became only minor way stations on the iron railroad of progress, through which the express train of medical science could rush with only a blast of a whistle to warn the loiterers to get out of its way. In more than a metaphorical way, the emperor had arrived on that train.
Recall that when Koch returned from Egypt and India proclaiming that he had discovered the cholera bacillus, there was indeed room for doubt. Koch had not satisfied his own postulates—no animal could be induced to fall sick with cholera—and epidemiological mysteries remained. (When Koch won the Nobel Prize in 1905, the citation was for his discovery of the tuberculosis bacillus, the more complete demonstration of his method.) Kaiser Wilhelm’s proclamation of Koch’s success was a gamble on science, in the service of imperial politics—he was strenuously seeking to catch up with the other European colonial powers. Seeking what he later called Germany’s “place in the sun” he had convened the Berlin Conference that divided Africa among them; his rush to industrialization was gathering pace; his unification of the disparate administrations across the patchwork quilt that had been the principalities, city-states, feudal, and episcopal estates of the former Holy Roman Empire was still incomplete.
At this time and in this context, tropical disease was a huge impediment to colonization, while medicine, especially in France, was justification for empire. The canonization of Koch was a triumph for German medical science, instantly making his laboratory a peer of France’s Pasteur Institute. Then as now, scientific competition was interwoven with geostrategic rivalry; it was a matter of both prestige and imperial capability. (France won a minor victory with the name of Pasteurella pestis.) Health administration, with its requirements of a unified census, border controls, and the machinery of case notification—issuing certificates of good health—required and justified a centralized bureaucracy. Infectious disease reporting and control was not a matter that could be left to the discretion of cities or baronies; unless all parts of the body politic conformed to the same central protocol, the health of the whole would be vulnerable to the deficiencies of its weakest part.
We can see now that Koch’s achievement was both scientific and rhetorical. His first scientific achievement was identifying the lifecycle of anthrax, but unable to specify the causal mechanism, he resorted to the persuasive metaphor of “host” and “parasite.” He went on to characterize the cholera vibrio as an “invader.” And—especially salient with respect to the rivalry between Berlin and Hamburg—the germ theory of infection was the charter for military centralism over laissez faire minimal government. On the train from Berlin arrived not just Koch but a freight of martial metaphor, mindset, and mobilizing capacity.
Medicine and the military are indeed deeply entangled throughout recorded history. Armies were epidemics on the march; regiments were depleted more by infection than battle; sailors fell victim to nutritional deficiencies such as scurvy. The scandalous hospital conditions for soldiers during the Crimea War of the 1850s were the occasion for Florence Nightingale to establish British nursing. Biological warfare has long been attempted, though historic successes were due more to chance than design. One account of the plague’s entry into Europe was that the Mongol army besieging the Crimean town of Kaffa used catapults to fling infected corpses into the city. The story of the gruesome projectiles may be true, but that is not how plague is transmitted. The Spanish conquest of Mexico was incalculably aided by smallpox, which stowed away on the conquistadors’ ships and killed as many as half of the immunologically naïve native Americans in its first and most deadly epidemic, while leaving the invaders—their faces pockmarked from earlier, immunity-inducing infections—untouched.
None of the above, however, imposed a military model on medicine itself. This changed with the application of modern industrial modes of organization to the organization of war, with the U.S. Civil War and the Franco-Prussian War. These were also the occasions on which modern medicine and the arsenal of epidemic control measures were applied to the same end. Tools of surveillance, standardization, and regimentation were applied equally to state-making, imperial expansion, industrial warfare, and population health. Just as war became about more than conquest, public health was never just about public health.
So too with Koch’s visit to Hamburg. The elders of the city had reason to fear that cholera control would jeopardize not just their commerce but also their prized constitutional autonomy. Over the previous decades, while the British empire had tried to balance health-based controls with free trade, the French had been much more assertive in using the anti-infection arsenal in the service of expanding the writ of the colonial state. The historian Patrick Zylberman recounts how the French government portrayed the disease as an “invasion” from the Levant and India, which justified martial medical measures and the establishment of the outer ramparts of Europe’s sanitary frontier in the Middle East.
The authorities in France’s Mediterranean ports didn’t want to require health inspections on arrival, so Paris assembled a coalition of European governments that imposed a regime of health inspection and oversight on the Ottoman Empire. So, even while the Ottomans were nominally independent, western European health officers were stationed in Cairo and Constantinople with the authority to control the westward departure of ships. Zylberman makes the point that the threat of cholera was sufficient justification for “pre-emptive intervention” in the eastern Mediterranean and even beyond: the Ottoman state was the “sick man of Europe” in two senses of the phrase, and the imperialists were already sinking their teeth into its weakening body. Whatever their geostrategic rivalries, Paris and Berlin saw the microbial threat from the east in a similar way: Germany imposed comparable measures along its long land frontiers.
In Hamburg in August 1892, worries about Berlin’s militaristic rule and the loss of long-cherished liberties were, of course, less pressing than the terrifying scourge in the water supply. Koch did not declare “war” on the vibrio, and his comparison of the overwhelmed Hamburg hospitals to a “battlefield” was as far as his military metaphors went. Nowhere in the debates of the day do we read political rhetoric of bodily integrity and decay, infection and purification, that was adopted by the Nazis a generation later. But as the militarized Prussian state took over the administration of Hamburg, starting with its hospitals and water supply, the corner was turned.
In the end Koch triumphed over von Pettenkofer; the biomedical paradigm shifted. Centralizing, authoritarian Prussia absorbed liberal Hamburg; Germany’s governance system consolidated. Less noticed, the military model of public health became hegemonic. The United States, which watched Hamburg closely—it was, after all, the port where the largest number of immigrants embarked—somehow managed this paradox. The U.S. Army Corps of Engineers became the principal weapon fighting Yellow Fever, in Cuba, Louisiana, and Panama alike, while generations of voters have rejected social medicine, as either a luxury the country cannot afford or as one step short of totalitarianism.
The metaphor of “fighting” a disease, apt for the body’s immune response to a pathogen, is incongruous for the social response to an epidemic. Nonetheless, the language of has become so familiar today that it is adopted unreflectingly—a mark of true hegemony. The traffic in metaphors runs both ways. When mobilizing for war or authoritarian measures, political leaders inveigh against “infestation” by invaders or infiltrators that are akin to pathogens. In times of health crisis, they like to “declare war” on a microbial “invisible enemy.”
The U.S. army medical and engineering corps earned their place in the annals of public health with meticulous research into Yellow Fever transmission followed by rigorous enforcement of programs of draining, capping, oiling standing water in wells, cisterns, tanks, pools, and use of insecticides to eradicate mosquito-breeding sites. In modern times, and especially since the post 9/11 anthrax scare raised the specter of bioterrorism, so deeply has the U.S. Department of Defense bored into all aspects of U.S. foreign policy that the instrument of choice in responding to diverse crises around the world, including epidemic disease, is the military. The army were the first international providers of relief to Indonesia after the tsunami of 2004 and to Haiti after the earthquake of 2010. President Barack Obama dispatched the 101st Airborne to “fight” Ebola in West Africa in 2014. Today, the National Guard and the U.S. Navy at the forefront of the COVID-19 emergency response. Military logistics appear to be indispensable in filling the gap of an under-provisioned emergency public health service.
However, recognizing the important operational role of the military in epidemic response shouldn’t seduce us into thinking that security officers and generals should be running the show. The American Civil Liberties Union was alive to this danger, warning in a 2008 report that coercive, law enforcement approaches would be counterproductive as well as dangerous to rights. Unsurprisingly, the potential for assuming war-time emergency powers and deploying security technologies is attractive to many political leaders precisely because of their dual usage. President Donald Trump has decided to call himself as a “wartime president.” He is following French President Emmanuel Macron, who declared “war” on the virus. In Italy, it is more of a police operation. Hungary’s Viktor Orbán has passed a law allowing him to rule by decree indefinitely and is blaming the pandemic on immigrants and refugees. In China, the lockdown is enforced by a combination of high-tech surveillance and old-fashioned Communist Party neighborhood mobilization—a “grid reaction.” In Israel, the government is proposing to deploy tracking technologies designed to follow terrorists against people believed to be infected with coronavirus. The Economist has coined the word “coronopticon” for such all-pervasive surveillance.
Activist reformers and silent revolutionaries
The wave of repressive measures enacted in response to COVID-19 would come as no surprise to the cast of our Hamburg drama. Europe’s nineteenth-century cholera epidemics marched in synchrony with its revolutions, notably in 1830–32 and 1848. “Cholera riots” were widespread. In 1892 mobs rampaged through the Russian cities of Astrakhan, Tashkent, Saratov and Donetsk. The cries of the afflicted provide the chorus to the protagonists, with a handful of spokesmen’s voices audible above the shouts and cries. But we would listen in vain for socialist revolutionaries.
Karl Marx was lodging at 28 Dean Street in Soho in 1854, five minutes’ walk from the famed Broad Street pump (according to Google Maps) and a minute from the nearest black (infected) dot on John Snow’s map in Meard Street. But he made only passing reference to the outbreak in his correspondence with Friedrich Engels, blaming it on poor housing. Engels had done the same in his 1845 book The Conditions of the Working Class in England, and in his preface to the 1892 edition added the line:
Again, the repeated visitations of cholera, typhus, small-pox, and other epidemics have shown the British bourgeois the urgent necessity of sanitation in his towns and cities, if he wishes to save himself and family from falling victims to such diseases. Accordingly, the most crying abuses described in this book have either disappeared or have been made less conspicuous.
Engels, it seems, quietly concedes that public health is a bourgeois science, and an effective one. For the communists, war and class war were the locomotives of history, and microbes had merely hitched a ride. As the historian Samuel Cohn observes, this is a baffling surrender of a political battlefield where they could have outflanked their class enemies. “An analysis of cholera and its social consequences did not enter any of Marx’s works published in his lifetime,” he notes, “and he appears to have been oblivious to any manifestations of its social protest and class struggle.” He continues:
Still more surprising is an absence of attention to cholera’s social violence by more recent historians of the New Left who have studied nineteenth- and twentieth-century class struggle meticulously—E.P. Thompson, Eric Hobsbawm, John Foster, John Calhoun, and others—despite these events sparking crowds estimated as high as 30,000, taking control of cities (even if only briefly), murdering governors, mayors, judges, physicians, pharmacists, and nurses, destroying factories and towns.
The oversight has begun to be remedied. Postcolonial historians and medical anthropologists have explored local resistance to colonial health policies and the suspicions that surround, among other things, polio vaccination programs. But still there is relatively little research on resistance to public health measures during epidemic emergencies. This is a gap, because each historical visitation of epidemic disease and its corresponding government measures was met with innumerable acts of everyday evasion and noncompliance.
In Italy in the sixteenth and seventeenth centuries, and most memorably in London in 1665, chroniclers of the plague have written about the reckless indifference of poor people to the dangers of contagion, and their subversion of whatever sanitary measures were imposed upon them. Daniel Defoe, like others who wrote on this subject, attributed this behavior to illiteracy, obstinacy, and fatalism. It may also have been a preference for accepting uncertainty (the lottery of the microbe) over the predictable hardship (destitution by unemployment). There are also intriguing echoes with colonized people’s resistance to imperial health and environmental diktat, which was usually arbitrary, unscientific, and often achieved nothing beyond a display of state power.
The nineteenth-century socialists’ silence on public health is doubly puzzling because their rivals on the left, the radical democrats were vocal. In the 1848 “springtime of the peoples,” while Marx and Engels were writing the Communist Manifesto, a young physician named Rudolf Virchow (1821–1902) was compiling a report on an outbreak of typhus in Silesia. Virchow came to be known both as the father of pathology and the founder of social medicine, but he was also a pioneering physical anthropologist; his studies of the size and shapes of the crania of different people made him conclude that there was no scientific basis for claims of racial superiority or inferiority. His medical practice radicalized his politics; his report on Silesia argued that medical interventions alone had little value, but rather social advancement through education, democracy and prosperity. Virchow joined the 1848 uprisings as a democrat with the slogan, “Medicine is a social science, and politics is nothing but medicine at scale.”
Like many erudite men of science of the era, Virchow’s medical views are hard to classify today. He was generally sympathetic to von Pettenkofer, though disagreed with him on cholera which he considered a contagion; he admired Koch, though oddly enough, disputed the role of the tuberculosis bacillus. Fundamentally, Virchow was a libertarian who believed that democracy, education and progress would eliminate disease. Evans, in Death in Hamburg, credits him with the crucial insight: “What Virchow’s theories made explicit was the indissoluble connection between medical science, economic interest, and political ideology.”
Virchow’s voice in the Hamburg chorus poses questions that resonate today. Contemporary liberals (in the U.S. usage of the word) are discomfited by the politics of pandemic. They lean toward social health on the grounds of equity but shudder when epidemiological risk management through quarantine and travel restrictions aligns with racist exclusionary policies. American liberals are reassured by the civil servants dedicated to science—Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, is today’s paragon of the virtuous deep state—but disturbed by the totalitarian implications of disease surveillance and control. The infection-control state is Max Weber’s military-bureaucratic state on steroids, requiring uniform sanitary habits throughout the population.
In his book, Disease and Democracy (2005), Peter Baldwin, describes how, in the later twentieth century, as chronic, non-infectious, and “lifestyle” diseases took over from infectious diseases as the main threats to health in industrialized countries, responsibility for health was shifted from states to citizens: “every man his own quarantine officer.” Baldwin poses the key question: “Can there be a democratic public health?” He doesn’t think so: “In the era of governmentality, public health remains one clear area of statutory control where the average law-abiding citizen might expect to feel the iron first through the velvet glove.”
Baldwin’s skepticism was a riposte to AIDS activists who believed that their own mobilization against the “gay plague” had not only accelerated the science but bent the arc of political history towards emancipation. President Ronald Reagan initially ignored the AIDS outbreaks among gay men, Haitians, and hemophiliacs, and was deaf to the demands of AIDS Coalition to Unleash Power, whose acronym ACT UP reflected their methods. Finally his Surgeon General C. Everett Koop, a fully credentialed conservative, and Anthony Fauci, just appointed to the job that he holds today, convinced Reagan to act.

In May 1990, ACT UP mounted a protest at NIH to bring awareness to the public the biomedical research in combating HIV-AIDS. Image: NIH History Office / Flickr
The country’s HIV and AIDS policies, and subsequently global policies too, were unprecedented in the history of public health responses to an incurable, sexually-transmitted disease targeting stigmatized groups—the words “innocent victims” applied to hemophiliacs and children born with HIV were the exception that proved that initial rule. People living with HIV and AIDS became involved in medical trials and policymaking. Activists offered to trial new drugs, arguing that they had nothing to lose by shortcutting the usual safety testing. They insisted on voluntary and confidential testing to protect their rights. In Africa government responses often ceded the agenda to civil society organizations and invariably included them in planning, and the international agencies set up to respond—UNAIDS and the Global Fund to Fight HIV/AIDS, Tuberculosis and Malaria—pioneered a model of global health governance based on human rights and inclusion.
Why epidemiologists should think like communities
I had a walk-on role late in the HIV and AIDS drama, in collaborative research on the politics, security and social aspects of the pandemic. And, writing in the spirit of Virchow, I insisted that there can only be a democratic public health. Like many others, I was inspired by the physician and medical anthropologist Paul Farmer; his book Infections and Inequalities (1999) is a manifesto for a partnership between social medicine and radical politics. The associations between poverty, inequality, and ill health and exposure to epidemics are well established and do not need to be emphasized here. Conscious of Aylward’s warning not to apply the “lesson” of the last epidemic to this one, I will make just one cautious, epidemiological point: there is in fact intriguing evidence that “people’s science” can play a crucial role in blunting epidemics and ensuring they don’t recur.
This is not to say we should romanticize folk medical wisdom: we shouldn’t. People’s epidemiology has more than its share of superstitions: numerous practices that are at best harmless and at worst dangerous or even fatal. Still, decades of people’s experimentation and observation have generated some real scientific breakthroughs, the emblematic example of which is smallpox variolation. An enslaved African American, familiar with the widespread African practice of injecting tissue from the pustules of smallpox patients into healthy individuals to produce a much less virulent version of the disease, introduced variolation to Massachusetts settlers in the early eighteenth century. Its efficacy was so convincing that George Washington inoculated his soldiers en masse. In 1798 the procedure was adapted by the English physician Edward Jenner in the form cowpox variolation, which he named vaccination.
There is also a demonstrable recent record of people’s science hastening the end of an epidemic. The case in point is Ebola in West Africa in 2014. Epidemiological models, which accurately charted the early, exponential growth phase of the epidemic, failed to predict its rapid decline. The models projected only burnout or a long taper as public health responses slowly reduced transmission, and not the remarkably rapid decrease that actually occurred. In his book Ebola: How a People’s Science Helped End an Epidemic (2016), the social anthropologist Paul Richards argues that the deficiency in the modeling is best explained by changes in intimate social behavior that could neither be captured by models nor even fully explained by people who were themselves altering the critical risk behaviors.
Anthropologists themselves didn’t connect the dots at the early stage of the outbreak. They had researched funerals and funeral rituals, but not the real danger point for contagion, which was the preparation of the body for burial. Family care for the sick was the other main context of transmission. Community health workers, social anthropologists, and epidemiologists had to speak to one another, understand each others’ knowledge, and find ways of communicating it. As Richards shows, the communities quickly learned to think like epidemiologists and adapted new safer body-handling practices, and the official top-down policies followed afterward. Post hoc modeling of the epidemic trajectory confirms that the best simulation of the decline is based on the widespread adoption of a community-based strategy for screening and travel restriction, which has the advantage that it requires a 50 percent compliance rate to be effective. The author of the review concludes, “We know of no other similarly validated explanation for the end of the outbreak.”
Each pandemic is different, but the logic of political action is much the same. Where political interests align with scientific advice, that advice becomes policy. This is where we can legitimately learn lessons. In the case of 1918, the lesson learned by the world leaders gathering to found the League of Nations was that international health is a problem that demands international cooperation. Smallpox was eradicated by exactly this sort of multilateral initiative in the 1970s. Measles, like smallpox, is caused by a virus that has only human hosts and so too could be eradicated, but to the wealthy nations that funded international health programs, it was regarded as harmless rite of passage for young children, even though it killed millions of them in poor countries every year. Because funds and political backing were available, the UN targeted polio instead: also a devastating disease but one far harder to eradicate, because the virus can exist in the wild.
In the case of HIV and AIDS, what “worked” was that pressure compelled governments to acknowledge their epidemic and respond, and public clamor forced pharmaceutical companies to bring down the cost of antiretroviral drugs so that treatment regimes at scale did not bankrupt African governments. Less unequivocally helpful was the pressure for strictly voluntary testing, which was codified as international best practice, even though compulsory or routine tests—in which the patient must specifically request not to be tested—could have helped prevent infections. And, as with any complex institution, political incentives came to align with the interests of the institution sometimes at the expense of the problem to be solved. The result was that the UN pushed for similar policies and metrics for every country, even though each individual country’s epidemic was different: some were centered on homosexual sex, others on heterosexual sex, yet others on intravenous drug use, and all had different social mores and networks. But it was simpler to standardize the package. In my book AIDS and Power (2006) I concluded that in African democracies, political incentives were structured to manage AIDS rather than to contain it: to provide treatment maximally and prevention barely sufficiently.
The 2003 SARS outbreak is the immediate precursor to COVID-19 in both pathogenesis and politics. It holds two political lessons. First, it shamed China’s government, but not enough. The government concealed the initial outbreak and reacted too late—the coronavirus spread across the world sparking local outbreaks, notably in Canada. Commentators speculated that SARS could be the crisis that cracked the Communist Party’s authoritarian control. In a volume reviewing the outbreak, Tony Saich asked whether SARS was “China’s Chernobyl or Much Ado About Nothing?” Saich reserved judgment, concluding that the Chinese authorities ought to learn. And seventeen years on, Saich’s assessment of the response to COVID-19 is “no, they didn't learn from the SARS epidemic.”
Implicit in this conclusion is that Premier Hu Jintao didn’t pay a political price for his flawed response to the disease. China developed its medical laboratories but did not create incentives for health workers to become whistleblowers: the default option for low-level officials receiving bad news was to please their superiors by insisting that all was still well. Second, the speedy suppression of SARS removed the market for pharmacological products that could treat coronaviruses or inoculate against them. Capitalism has no incentive for pre-emptively responding to a future global public bad (as the economists like to say).
From this we distill the elementary and wholly unsurprising lesson that well-articulated political demands shape the politics of public health. Democracies can demand public health.
In the next-to-last act of the Hamburg drama, Virchow ends the scene. He has already posed the key question—whether it was material interest, political ideology, or medical science that determined the outcome. And although none of the protagonists answered the question—neither the cholera vibrio, not von Pettenkofer and the city merchants and lawyers, not Koch and his Emperor, and not even the dissonant chorus—Virchow makes the claim that social emancipation and democracy will finally overcome cholera.
Thinking critically in a pandemic
What does all this mean for COVID-19? We face a new virus with uncertain epidemiology that threatens illness, death, and disruption on an enormous scale. Precisely because every commentator sees the pandemic through the lens of his or her preoccupations, it is exactly the right time to think critically, to place the pandemic in context, to pose questions.
The clearest questions are political. What should the public demand of their governments? Through hard-learned experience, AIDS policymakers developed a mantra: “know your epidemic, act on its politics.” The motives for—and consequences of—public health measures have always gone far beyond controlling disease. Political interest trumps science—or, to be more precise, political interest legitimizes some scientific readings and not others. Pandemics are the occasion for political contests, and history suggests that facts and logic are tools for combat, not arbiters of the outcome.
While public health officials urge the public to suspend normal activities to flatten the curve of viral transmission, political leaders also urge us to suspend our critique so that they can be one step ahead of the outcry when it comes. Rarely in recent history has the bureaucratic, obedience-inducing mode of governance of the “deep state” become so widely esteemed across the political spectrum. It is precisely at such a moment, when scientific rationality is honored, that we need to be most astutely aware of the political uses to which such expertise is put. Looking back to Hamburg in 1892, we can readily discern what was science and what was superstition. We need our critical faculties on high alert to make those distinctions today.
At the same time, COVID-19 has reminded a jaded and distrustful public how much our well-being—indeed our survival—depends upon astonishing advances in medical science and public health over the last 140 years. In an unmatched exercise of international collaboration, scientists are working across borders and setting aside professional rivalries and financial interests in pursuit of treatment and a vaccine. People are also learning to value epidemiologists whose models are proving uncannily prescient.
But epidemiologists don’t know everything. In the end it is mundane, intimate, and unmeasured human activities such as hand-washing and social distancing that can make the difference between an epidemic curve that overwhelms the hospital capacity of an industrialized nation and one that doesn’t. Richards reminds us of the hopeful lesson from Ebola: “It is striking how rapidly communities learnt to think like epidemiologists, and epidemiologists to think like communities.” It is this joint learning—mutual trust between experts and common people—that holds out the best hope for controlling COVID-19. We shouldn’t assume a too simple trade-off between security and liberty, but rather subject the response to vigorous democratic scrutiny and oversight—not just because we believe in justice, transparency and accountability, but also because that demonstrably works for public health.
As we do so, it is imperative we attend to the language and metaphors that shape our thinking. Scientists absorb (fundamental) uncertainty within (measurable) risk; public discourse runs along channels carved by more than a century of military models for infectious disease control. By a kind of zoonosis from metaphor to policy, “fighting” coronavirus may in the worst case bring troops onto our streets, security surveillance into our personal lives. Minor acts of corporate charity, trumpeted at a White House bully pulpit, may falsely appear more significant than the solidarities of underpaid, overworked health workers who knowingly run risks every day. Other, democratic, responses are necessary and possible: we need to think and talk them into being.
Perhaps the most difficult paradigm to shift will be to consider infectious agents not as aliens but as part of us—our DNA, microbiomes, and the ecologies that we are transforming in the Anthropocene. Our public discourses fail to appreciate how deeply pathogenic evolution is entangled in our disruption of the planet’s ecosystem. We have known for decades that a single zoonotic infection could easily become pandemic, and that social institutions for epidemic control are essential to provide breathing space for medical science to play catch-up. Our political-economic system failed to create the material incentives and the popular narrative for this kind of global safety net—the same failure that has generated climate crisis.
This is the final, unfinished act of the drama. Can human beings find a way to treat the pathogen not as an aberration, but as a reminder that we are fated to co-exist in an unstable Anthropocene? To expand on the words of Margaret Chan, WHO director at the time of SARS, “The virus writes the rules”—there is no singular set of rules. We have collectively changed the rules of our ecosystems, and pathogens have surprised us with their nimble adaptations to a world that we believed was ours.
Alex de Waal is Executive Director of the World Peace Foundation at the Fletcher School at Tufts University. He is the author of Mass Starvation: The History and Future of Famine, The Real Politics of the Horn of Africa: Money, War and the Business of Power, and editor of Advocacy in Conflict: Critical Perspectives on Transnational Activism.
While we have you...
...The Boston Review needs your help. Confronting the many challenges of COVID-19—from the medical to the economic, the social to the political—demands all the moral and deliberative clarity we can muster. In Thinking in a Pandemic, we’ve organized the latest arguments from doctors and epidemiologists, philosophers and economists, legal scholars and historians, activists and citizens, as they think not just through this moment but beyond it. While much remains uncertain, Boston Review’s responsibility to public reason is sure. That’s why you’ll never see a paywall or ads. It also means that we rely on you, our readers, for support. If you like what you read here, pledge your contribution to keep it free for everyone by making a tax-deductible donation.

Spread the word