The COVID-19 pandemic is continuing to have unusual and unexpected effects on a number of respiratory diseases — some have been quashed, others have ploughed through and still more are rebounding off-season. These fluxes are complicating medical responses to the pandemic, but also providing scientists with an opportunity to study how these viruses spread.
As cold-and-flu season ostensibly starts in the Northern Hemisphere, researchers warn to expect the unexpected. “If anyone tells you they know, they don’t know,” says epidemiologist John Paget at the Netherlands Institute for Health Services Research in Utrecht. Most agree that influenza will eventually rebound, possibly fiercely, as travel restrictions and societal interventions designed to curb the coronavirus, such as mask wearing, wane. “Once we let our good health practices lapse, then flu is likely to hit hard,” says Robert Ware, a clinical epidemiologist at Griffith University in Queensland, Australia.
Seasonal flu typically kills 290,000–650,000 people a year worldwide. But for most of 2020 and 2021, it practically vanished from much of the globe. FluNet, a tool for tracking global virological data on influenza maintained by the World Health Organization, shows that the proportion of positive flu tests has remained roughly flat since April 2020, despite increased surveillance (see ‘Viral shift’).
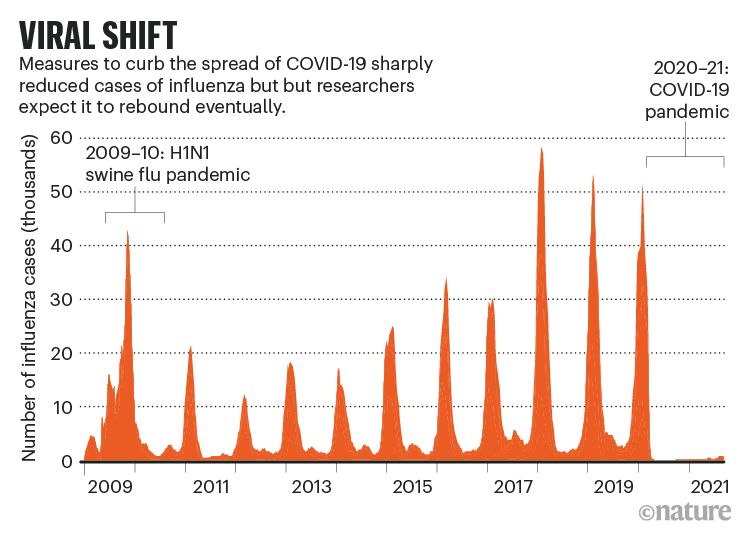
Source: World Health Organization
Flu break
The United States recorded just 646 flu deaths in the 2020–21 season — the annual average is in the tens of thousands — and there was only one paediatric flu death. Australia has had no seasonal influenza deaths so far in 2021, compared with between 100 and 1,200 in previous years.
The decline in flu has persisted despite the variable lifting of social interventions to curb coronavirus. This hammers home the importance of international travel in bringing flu to any given country, says Richard Webby at St. Jude Children’s Research Hospital in Memphis, Tennessee. “It says a lot about seeding events and how important they are,” he says. Flu has continued to circulate at low levels in the tropics, researchers note, so will probably spread from there once borders reopen.
Pandemic response measures also seem to have suppressed some bacterial infections, including those that cause pneumonia and meningitis and are associated sepsis1. But some viruses have behaved differently. Rhinoviruses, for example, a major cause of the common cold, continued to spread throughout the pandemic, and infections even shot up in some countries2, possibly because these viruses aren’t as susceptible as many others to measures such as surface cleaning and hand washing, and because they faced little competition from other respiratory viruses. There is emerging evidence that these mild viruses might protect people from more serious diseases during infection3,4.
And some typical winter viruses have bounced back out of season. Infections caused by common human coronaviruses (another major common-cold culprit) and parainfluenza viruses were at very low levels in the United States in 2020 but started to rise to pre-pandemic levels in spring 2021 — an unusual time for colds to hit. Likewise, infections with respiratory syncytial virus (RSV), which usually causes mild cold symptoms but is also responsible for about 5% of deaths in children under 5 worldwide, were at a historic low for a year and then started rising months later than usual, in April 2021. RSV infections were still climbing at the end of August (see ‘Strong rebound’).
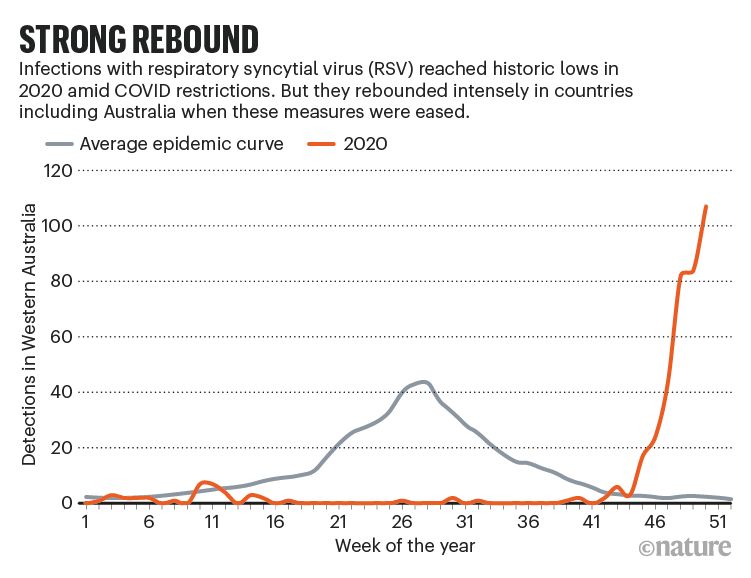
Source: Foley, D. A. et al. Clin. Infect. Dis. http://doi.org/10.1093/cid/ciaa1906 (2021).
Off-season peaks
The strangely timed bumps might be related to school reopenings, according to a report from the US Centers for Disease Control and Prevention (CDC)5, along with a build-up of susceptible, unexposed infants in the absence of a vaccine (RSV vaccines are under development).
Off-season RSV peaks have been seen elsewhere, too, in countries including South Africa, Japan, Australia and the Netherlands. In Western Australia, an RSV peak in December 2020 was 2.5 times larger than the July peak for 20196. A steep onset of disease doesn’t necessarily translate to more cases overall, however: the total number of RSV cases in Queensland was lower than usual, Ware notes, “but because all the cases came close together it was much more intense”, putting strain on health resources.
It would be worrying to see rebound effects caused by a build-up of immunologically naive people in seasonal flu, researchers caution. Around the world, there are signs of circulating H3N2, H1N1 and B influenza viruses, says Amber Winn, an epidemiologist in the CDC’s Division of Viral Diseases in Atlanta, Georgia. A wave of influenza B infections in winter 2019–20, she notes, contributed to a record number of paediatric flu deaths that season. “That’s why getting your flu vaccine this season may be especially important,” she says.
doi: https://doi.org/10.1038/d41586-021-02558-8
References
- 1.
Brueggemann, A. B. et al. Lancet Digital Health 3, E360–E370 (2021).
- 2.
Takashita, E. et al. Influenza Other Respir. Viruses 15, 488–494 (2021).
- 3.
Van Leuven, J. T. et al. Preprint at bioRxiv https://doi.org/10.1101/2020.11.06.371005 (2021).
- 4.
Dee, K. et al. J. Infect. Dis. 224, 31–38 (2021).
- 5.
Olsen, S. J. et al. Morbid. Mortal. Weekly Rep. 70, 1013–1019 (2021).
- 6.
Foley, D. A. et al. Arch. Dis. Child. https://doi.org/10.1136/archdischild-2021-322507 (2021).


Spread the word